Table of Contents
If you’ve ever caught yourself asking, “Why am I always tired?” even after a full night’s sleep, decent food choices, and trying to “do everything right”, you’re not alone. Persistent fatigue is one of the most common reasons people seek medical help, yet it’s also one of the most misunderstood symptoms.
Many people are told that since their blood tests are “normal,” it’s all in their head, that stress is to blame, or that tiredness is simply part of aging or a busy life. But feeling exhausted all the time isn’t a personal failure, and it isn’t something you should just push through. From a functional medicine perspective, chronic fatigue is often a signal, not a diagnosis.
This article explores the functional medicine approach to fatigue, helping you understand what your body may be communicating, why conventional answers sometimes fall short, and how a root-cause lens like the one used in the Hormone Reset framework can offer clarity without quick fixes or exaggerated claims.

Feeling Tired Is a Signal, Not a Diagnosis
In functional medicine, fatigue is viewed as a message from the body rather than a standalone condition. Instead of asking only “What label fits this symptom?”, the more useful question becomes:
“What systems might be under strain?”
Fatigue rarely has a single cause. It often reflects the combined effects of multiple factors like stress, sleep quality, nutrient status, blood sugar regulation, gut health, hormonal signaling, toxicity, and even how efficiently your cells produce energy.
This systems-based view is what differentiates always tired functional medicine thinking from symptom-focused care. The goal isn’t to dismiss conventional medicine, but to expand the lens when the usual explanations don’t fully match how someone feels.
The Hidden Energy System Inside Your Body
When people think about energy, they often think in terms of motivation or willpower. But biologically, energy starts at the cellular level.
When Cellular Energy Breaks Down
Inside nearly every cell are structures called mitochondria, often described as the body’s energy producers. They help convert food and oxygen into ATP, the molecule your body uses for energy. When mitochondrial efficiency is reduced, the result can feel like constant fatigue, even if sleep and calories are adequate.
This doesn’t mean something is “broken.” Reduced mitochondrial health has been associated with factors such as chronic stress, inflammation load, nutrient deficiencies, and ongoing immune activation. Over time, the body may conserve energy as a protective response, leaving you feeling low energy throughout the day.
Hormones, Stress, and the Exhaustion Loop
Hormones act as messengers, coordinating how different systems communicate. When this signaling becomes dysregulated, fatigue can be one of the earliest signs.
Cortisol and the “Wired but Tired” Pattern
Chronic stress, whether emotional, physical, or metabolic, can disrupt the body’s normal stress response. Instead of a smooth daily rhythm, cortisol levels may become imbalanced. Some people feel constantly “on edge” yet exhausted, while others struggle to get going in the morning.
In functional medicine, this is sometimes described as an adrenal fatigue pattern, not a formal diagnosis, but a way to describe how chronic stress may influence energy regulation.
Thyroid Function Beyond “Normal” Labs
The thyroid plays a key role in metabolic rate and energy production. Standard lab tests can fall within reference ranges while subtle functional changes still affect how someone feels. A hormone imbalance doesn’t always show up as a disease, but it can still contribute to fatigue.
This is where frameworks like Hormone Reset focus on understanding patterns and trends, rather than chasing isolated numbers.
Blood Sugar Swings That Drain Your Energy
Blood sugar regulation is another commonly overlooked contributor to fatigue. When glucose levels rise and fall rapidly, energy can feel unpredictable.
Some people notice crashes after meals, reliance on caffeine to function, or feeling shaky, irritable, or foggy between meals. These patterns don’t necessarily indicate diabetes, but they do point to challenges with blood sugar balance that can affect how steady your energy feels throughout the day.
Gut Health, Inflammation, and Fatigue
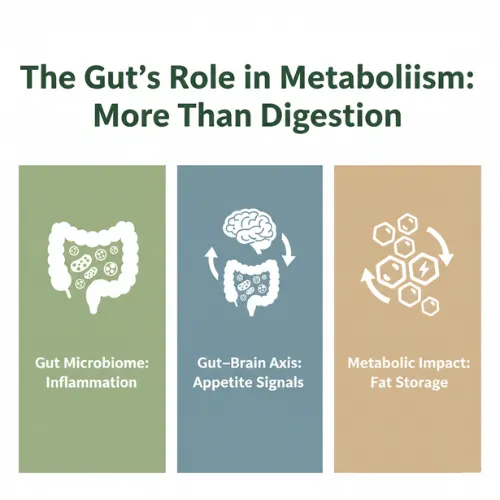
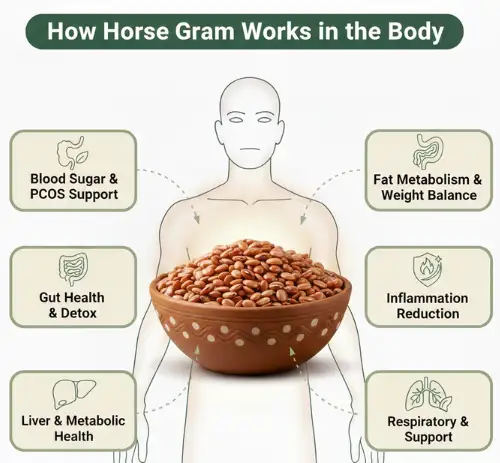
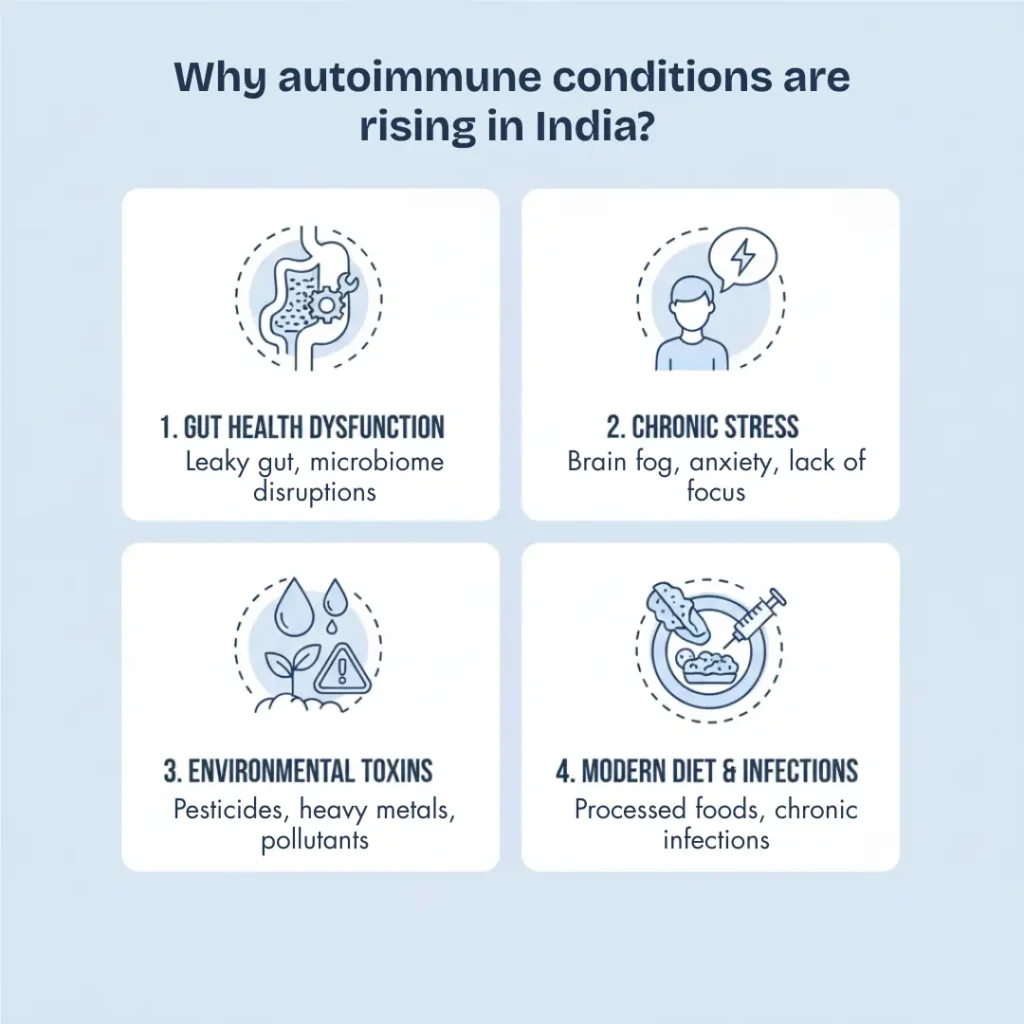
Your digestive system does far more than process food. It plays a role in nutrient absorption, immune regulation, and inflammation control, all of which influence energy.
When gut health is compromised, the body may struggle to absorb key nutrients or manage immune responses efficiently. Low-grade inflammation can increase the body’s energy demands, leaving fewer resources available for daily functioning.
Rather than blaming the gut as a single cause, functional medicine looks at how digestion, immunity, and energy metabolism interact.
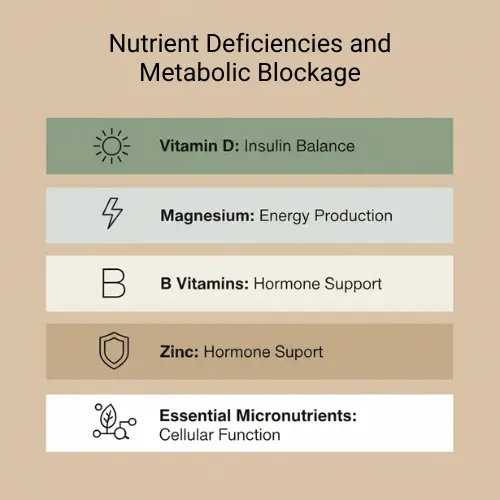
Nutrient Deficiencies That Quietly Exhaust You
Fatigue is commonly associated with nutrient deficiency, particularly involving iron, B-vitamins, magnesium, vitamin D, and CoQ10. However, deficiencies don’t always stem from poor intake alone.
Absorption issues, chronic stress, inflammation, medications, and individual biochemistry can all affect nutrient status. This is why a functional medicine approach emphasizes understanding why a deficiency exists, rather than simply recommending supplements.
Sleeping Enough but Still Exhausted
One of the most frustrating experiences is being exhausted even after sleep. In these cases, the issue is often sleep quality rather than quantity.
Factors such as circadian rhythm disruption, nighttime stress responses, mood disorders, or breathing disturbances can all interfere with restorative sleep. Poor sleep doesn’t just leave you tired the next day—it can compound fatigue by affecting hormones, blood sugar, and inflammation.
When “Normal” Tests Don’t Explain How You Feel
Many people who ask “Why am I tired all day?” have already undergone testing, only to be told everything looks fine. This is where frustration often peaks.
Conventional labs are designed to detect disease, not necessarily early dysfunction. Functional medicine doesn’t reject these tests; it builds on them by considering optimal ranges, symptom patterns, and additional assessments when appropriate.
This is often where functional medicine for fatigue becomes valuable: not because it replaces standard care, but because it offers a broader context for interpreting results.
A Functional Medicine Roadmap to Reclaim Energy
A functional medicine approach to fatigue focuses on personalization. Rather than applying a single protocol, it aims to understand which systems are most relevant for each individual.
This may involve:
- identifying stress and hormone patterns
- supporting metabolic and mitochondrial health
- improving sleep and circadian rhythm
- addressing gut-related inflammation
- restoring nutrient balance gradually
Approaches like Hormone Reset emphasize sustainable, step-by-step support rather than aggressive interventions. The goal is long-term resilience, not short-term stimulation.

Daily Habits That Actually Restore Energy
If you’re constantly wondering, “Why do I feel exhausted all the time?”, the answer isn’t in pushing harder—it’s in resetting the systems that generate sustainable energy. Functional medicine, particularly approaches like Hormone Reset, focuses on understanding your body’s signals and supporting natural rhythms instead of masking fatigue with stimulants.
Align Your Hormonal Rhythms
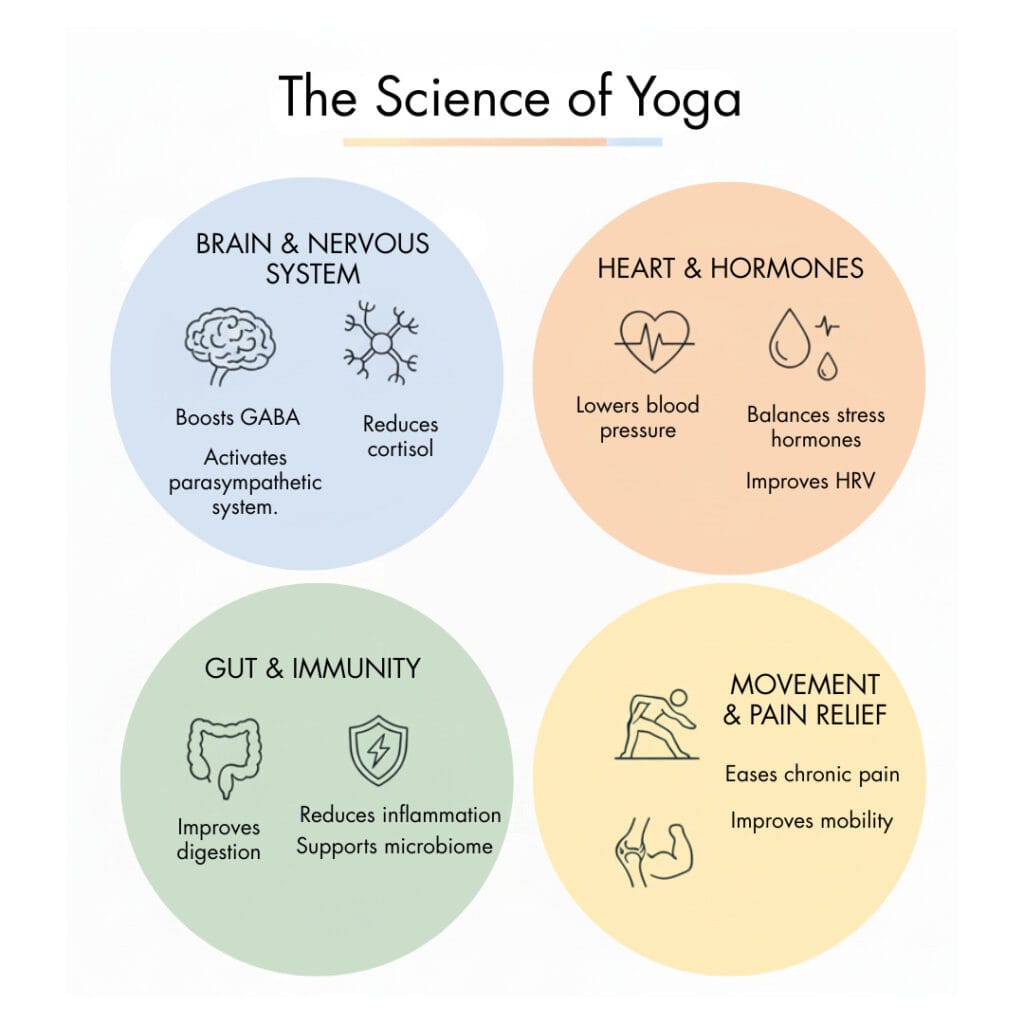
Start by paying attention to your hormonal patterns. Early morning exposure to natural light helps cue cortisol release, setting your circadian clock for alertness in the morning and restful sleep at night. Going to bed and waking up at consistent times reinforces these patterns, signaling your body when to release energy and when to recharge. Tracking energy peaks across the day allows you to schedule tasks in alignment with your natural highs and lows, so you work with your physiology, not against it.
Nourish Steady Energy Through Food
Nutrition plays a central role in maintaining consistent energy. Meals that combine protein, healthy fats, and fiber stabilize blood sugar, preventing mid-morning or mid-afternoon crashes. Highly processed carbs and sugar spikes can drain energy, while light, strategically timed snacks support metabolism without overloading digestion. Functional medicine emphasizes tailoring eating patterns to your unique energy rhythms, creating steady fuel throughout the day.
Boost Cellular Power
At the core of energy production are your mitochondria, the tiny cellular engines that convert food into usable energy. Adequate levels of magnesium, B vitamins, CoQ10, and vitamin D support these processes. Gentle movement, such as a brisk walk, yoga, or light resistance exercises, stimulates mitochondrial efficiency without adding fatigue. The key is to move when your energy naturally peaks, optimizing cellular function without overtaxing your body.
Support Gut Health
Your gut directly affects how energized you feel. Anti-inflammatory foods, colorful vegetables, healthy fats, and fermented foods support a balanced microbiome, which aids nutrient absorption and regulates low-level inflammation. Proper hydration enhances digestion and nutrient delivery, while mindful eating, chewing slowly, and avoiding late-night heavy meals reduces digestive strain and prevents post-meal sluggishness.
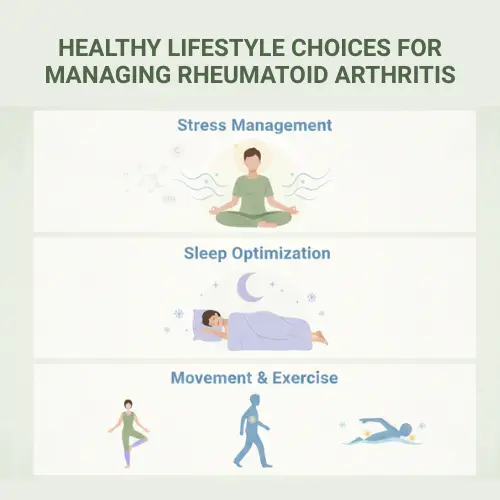
Manage Stress and Protect Energy
Chronic stress can silently drain energy. Functional medicine encourages small, intentional resets throughout the day—like deep breathing, meditation, or brief grounding exercises to calm the nervous system and regulate cortisol levels. Pausing strategically allows your body to recover, creating a more sustainable rhythm of alertness and rest. Pacing tasks according to natural energy highs and lows helps preserve stamina and avoid burnout.
Why This Works
By integrating these approaches, a Hormone Reset framework addresses fatigue at the root. It supports energy across hormones, mitochondria, gut function, blood sugar, and stress regulation. Over time, these shifts help your body move from chronic exhaustion to steady, reliable vitality without caffeine, extreme routines, or quick-fix hacks.
Client Testimonials
Anitha M
“I am very glad to take up my health improvement journey with Hormone Reset. I had really bad skin irritation, Barrett’s esophagus, and low energy levels. They were addressed in a systematic way, and the issues are gradually coming down. I can see my energy levels improving, and plan to continue further. Thanks to the clinician, Ruhi Mam, and Siddharth Sir.”
Sahana Adhikari
“The Hormone Reset program was very helpful to me. I joined it hoping to lose weight, but what I gained was a holistic approach to life and, most importantly, more energy. Dr. Ruhi, Siddharth, and their team were always there to answer any doubts or questions I had. They started with a comprehensive blood test, including a NutriFit test, and prepared a complete diet-cum-healing plan. The weekly group sessions were motivating and helped me stay on track. As a result, my sleep improved, muscle cramps stopped, and I feel energetic throughout the day.”
FAQs: Understanding Fatigue & the Hormone Reset Approach
1. Why do I feel tired even after a full night’s sleep?
Feeling exhausted despite adequate sleep often points to underlying system imbalances rather than poor sleep alone. Factors like hormone dysregulation, blood sugar swings, nutrient deficiencies, mitochondrial efficiency, and low-grade inflammation can all impact energy levels. The Hormone Reset program looks at these root causes to restore sustainable energy.
2. Can normal blood tests rule out the cause of my fatigue?
Not always. Standard lab tests detect disease but may miss early functional imbalances. Functional medicine evaluates patterns, optimal ranges, and additional assessments, helping uncover subtle issues that affect energy, like thyroid function, adrenal signaling, or nutrient absorption.
3. How can hormones affect my energy levels?
Hormones act as messengers that regulate metabolism, sleep, and stress responses. Imbalances in cortisol, thyroid hormones, or other signaling pathways can leave you feeling “wired but tired” or sluggish. Addressing these patterns, rather than just treating symptoms, is key to restoring steady energy.
4. What lifestyle changes help improve energy naturally?
Sustainable energy comes from supporting the body’s natural rhythms. Functional approaches include aligning sleep-wake cycles with circadian rhythms, stabilizing blood sugar through balanced meals, boosting mitochondrial health with proper nutrition and gentle movement, managing stress through mindful practices, and supporting gut health for optimal nutrient absorption.
Reframing Fatigue: Listening to What Your Body Is Asking For
Feeling tired all the time isn’t something you’re meant to ignore, normalize, or push through with willpower. Fatigue is one of the body’s most honest signals—a quiet request for support when systems are under strain. When energy is low, it’s rarely about laziness or lack of discipline. More often, it reflects how deeply interconnected your hormones, metabolism, stress response, gut health, and sleep truly are.
A functional medicine perspective invites a shift in mindset. Instead of asking, “How do I get more energy right now?”, the better question becomes, “What is draining my energy in the first place?” This reframing creates space for understanding rather than self-judgment, and for sustainable change rather than temporary stimulation.
Fatigue doesn’t define you, and it isn’t something you have to accept as “normal.” Through a thoughtful Hormone Reset approach, what once felt like endless exhaustion can become a signal guiding you toward greater awareness, smarter support, and long-term vitality.

References
- Why You’re Always Tired: A Functional Medicine Perspective -California Center for Functional Medicine
- Why Am I Always Tired? Functional Medicine Has Clues – Docere Integrated Medicine
- A Functional Medicine Approach to Fatigue – Rupa Health
- Tired All the Time? How Functional Medicine Identifies Hidden Causes of Fatigue-Salina Chiropractic
- Why am I so tired? How Functional Medicine Answers this Common Question -Jester Family Chiropractic
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset