Table of Contents
Introduction: Understanding Stomach Gas from a Functional Perspective
Stomach gas, bloating, and digestive discomfort are common complaints that many people experience after meals. While occasional gas is normal, persistent or excessive gas signals that the digestive system is under stress or not functioning optimally. Conventional advice often focuses on temporary relief, such as over-the-counter medications or lifestyle clichés like “eat smaller meals” or “drink water during meals.”
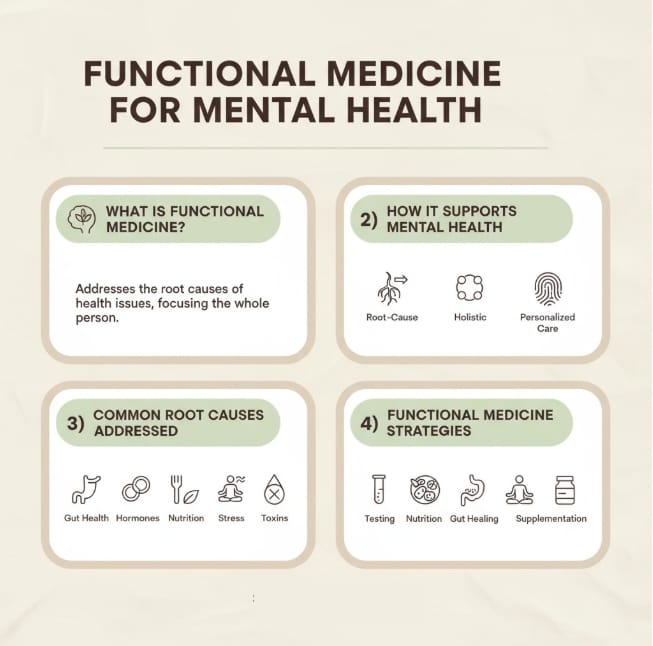
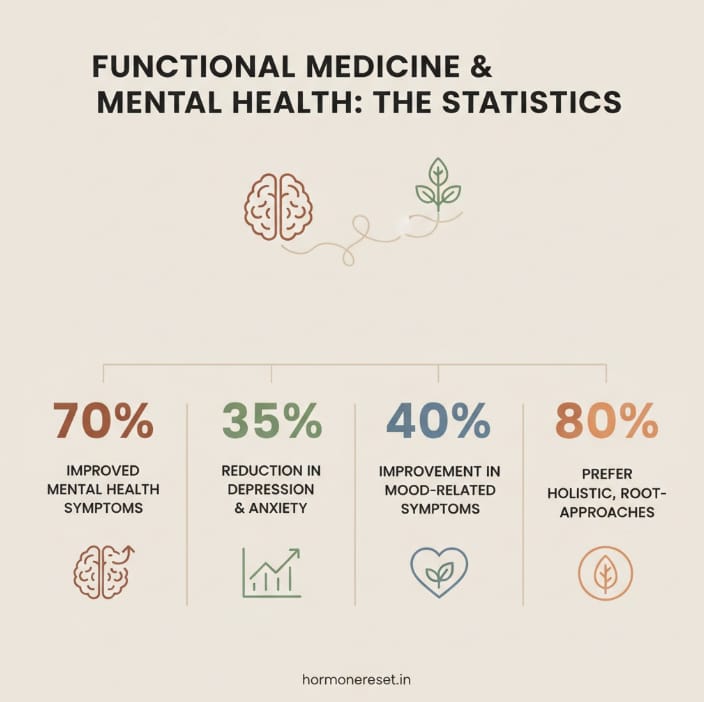
From a Functional Medicine perspective, gas is not an isolated problem—it is a symptom that points to deeper imbalances in the digestive system. Understanding why gas occurs, rather than just masking it, is key to long-term digestive comfort. Gas typically arises from bacterial fermentation in the gut, impaired motility, enzyme deficiencies, microbiome imbalances, and food sensitivities. By addressing these root causes, you can achieve both immediate relief and sustained improvement in digestive health.
What’s Really Happening in Your Gut
Excess stomach gas is rarely just a minor nuisance—it usually reflects deeper digestive imbalances. The main contributors include bacterial fermentation of undigested food, an imbalanced gut microbiome, insufficient digestive enzymes, slow gut motility, and individual food sensitivities. Understanding and addressing these root causes is key to achieving lasting relief and optimal digestive health.
Fermentation by Gut Bacteria
The most significant source of stomach gas is the fermentation of undigested carbohydrates by gut bacteria. When food is not fully broken down in the small intestine, it reaches the colon where bacteria metabolize it, producing gases such as hydrogen, methane, and carbon dioxide. This process can create the familiar sensations of bloating, pressure, and abdominal discomfort.
Factors that increase bacterial fermentation include:
- Incomplete digestion of carbohydrates due to low stomach acid or insufficient digestive enzymes.
- Overgrowth of gas-producing bacteria in the small intestine or colon.
- Consumption of high-FODMAP foods like beans, lentils, onions, garlic, and certain fruits, which ferment more readily.
Bacterial fermentation is a natural process, but excessive or poorly timed fermentation leads to uncomfortable gas buildup.
Imbalance in Gut Microbiome (Dysbiosis)
A healthy gut microbiome maintains digestive balance, aids nutrient absorption, and prevents overproduction of gas. Dysbiosis, or an imbalance between beneficial and harmful microbes, is a common underlying factor for chronic bloating.
Causes of dysbiosis include:
- Repeated antibiotic use
- High-sugar or ultra-processed diets
- Chronic stress
- Sedentary lifestyle
Certain bacteria, such as methane-producing archaea or sulfur-producing microbes, generate significantly more gas than others. When these bacteria dominate, even normal meals can lead to discomfort.
Poor Digestion or Enzyme Deficiency
Effective digestion relies on stomach acid, digestive enzymes, and bile to break down carbohydrates, fats, and proteins. When any of these components are insufficient, food passes into the intestines partially undigested, creating a perfect substrate for gas-producing bacteria.
Common contributors include:
- Low stomach acid (hypochlorhydria)
- Inadequate pancreatic enzyme activity
- Reduced bile secretion
- Gut inflammation that impairs nutrient absorption
Supporting digestion through proper enzyme activity and stomach acid balance reduces substrate for fermentation and minimizes gas formation.
Slow Gut Motility
When food moves too slowly through the digestive tract, fermentation increases, and gas has more time to accumulate. Slow motility can be caused by:
- Chronic stress or sympathetic nervous system activation
- Low thyroid hormone levels
- Nutrient deficiencies s,uch as magnesium or B12
- Lack of physical movement
Functional Medicine emphasizes restoring natural gut motility rather than relying on frequent meals, which can disrupt the Migrating Motor Complex (MMC)—a critical wave that clears the small intestine of bacteria and leftover food.
Food Intolerances and Sensitivities
Certain foods are more likely to cause gas in sensitive individuals. Common triggers include:
- Dairy (lactose intolerance)
- Gluten
- Beans, lentils, and chickpeas
- Onions, garlic, and other high-FODMAP vegetables
- Sugar alcohols found in processed foods
When these foods are consumed, undigested carbohydrates ferment rapidly, producing gas and bloating. A structured elimination and reintroduction approach can help identify personal triggers.

Recognizing When Stomach Gas Becomes a Concern
Occasional gas is a normal part of digestion, but frequent or severe bloating may interfere with daily life. Signs that stomach gas requires attention include:
- Bloating that appears 30–60 minutes after meals
- Chronic abdominal fullness or pressure
- Excessive burping or flatulence
- Discomfort that affects social situations or daily activities
- Gas accompanied by changes in bowel habits, pain, or unexplained weight loss
Persistent gas is a signal that deeper digestive imbalances need to be addressed rather than ignored.
Functional Medicine Strategies for Quick Gas Relief
While root-cause management is the long-term solution, there are effective methods to relieve discomfort naturally in the short term:
Gentle Movement and Stretching
- Light walking after meals helps stimulate gut motility and reduce bloating.
- Yoga poses like Knee-to-Chest (Apanasana) and Child’s Pose gently shift trapped gas and relieve pressure. Hold each pose for 30–60 seconds.
Deep Breathing and Relaxation
- Controlled, diaphragmatic breathing relaxes the abdominal muscles and supports natural gas passage.
- Stress reduction techniques such as mindfulness or progressive relaxation help normalize digestive rhythm.
Warm Herbal Beverages
- Peppermint tea: Relaxes intestinal muscles, allowing gas to pass more easily.
- Ginger tea: Reduces bloating, eases abdominal discomfort, and stimulates digestion.
- Chamomile tea: Calms the stomach and nervous system, indirectly supporting gas relief.
Sipping slowly allows the digestive system to respond effectively.
Eating Habits That Support Digestive Comfort
Food Choices
- Choose low-FODMAP foods such as rice, zucchini, carrots, and certain fruits to reduce fermentation.
- Replace high-gas foods like beans, onions, and cruciferous vegetables with gentler alternatives.
- Use lactose-free or plant-based dairy if sensitive to lactose.
Mindful Eating
- Eat slowly and chew thoroughly to reduce fermentation caused by undigested food.
- Avoid talking while eating and minimize distractions like phones or screens.
Meal Timing and Hydration
- Avoid frequent snacking that disrupts gut motility.
- Sip water between meals rather than drinking large amounts with food
- Focus on gradual, consistent hydration to support smooth digestion.
Lifestyle Practices for Long-Term Relief
In Functional Medicine, digestion is not viewed in isolation; it is intimately connected with broader lifestyle factors. Physical activity plays a vital role in supporting gut motility, helping food move efficiently through the digestive tract and reducing the risk of excessive fermentation and gas buildup. Gentle walks after meals or light stretching can stimulate natural digestive rhythms and ease bloating. Equally important is stress management, as chronic stress activates the sympathetic nervous system and slows digestion, creating an environment where gas and bloating are more likely. Techniques such as deep breathing, meditation, or short mindful breaks throughout the day can help relax the body, promote efficient motility, and reduce abdominal discomfort. Posture and physical comfort also contribute to digestive ease; sitting upright during meals ensures proper organ alignment and allows the digestive system to function optimally, while wearing non-restrictive clothing reduces unnecessary pressure around the abdomen. Finally, maintaining consistent daily routines—such as getting adequate sleep, eating dinner at regular times, and avoiding late-night snacking—supports the natural circadian rhythms of the gut. Together, these lifestyle strategies enhance digestion, support the microbiome, and reduce the frequency and severity of bloating and gas over time.
When to Seek Medical Advice
While most gas and bloating can be managed through diet, lifestyle, and functional strategies, persistent or severe symptoms may indicate underlying medical conditions that require professional evaluation. It is important to seek medical attention if gas is accompanied by intense abdominal pain, persistent vomiting, diarrhea, or noticeable changes in bowel movements such as blood in the stool or black, tarry stools. Unexplained weight loss alongside bloating or gas can also signal a deeper digestive issue that should not be ignored. In these cases, a healthcare professional may recommend targeted testing to uncover the root cause, such as comprehensive stool analysis to evaluate microbiome balance, digestive enzyme function, or inflammation; SIBO breath tests to detect bacterial overgrowth in the small intestine; food sensitivity panels to identify triggering foods; and nutrient deficiency assessments to ensure the body is receiving essential vitamins and minerals for optimal digestion. Identifying the underlying cause through these functional tests allows for a personalized approach, addressing the source of excessive gas rather than just managing symptoms, and provides a path toward lasting digestive wellness.
FAQs: How to Ease Stomach Gas Naturally and Feel Comfortable
1. What is the main cause of stomach gas?
The primary cause of stomach gas is bacterial fermentation of undigested carbohydrates in the gut. When food is not fully broken down in the small intestine, it reaches the colon where gut bacteria metabolize it, producing gases such as hydrogen, methane, and carbon dioxide. Factors like slow gut motility, enzyme deficiencies, or an imbalance in the gut microbiome can worsen fermentation, leading to bloating and discomfort. While swallowing air can contribute slightly, it is rarely the main driver of chronic gas.
2. Which foods are most likely to cause gas and bloating?
Certain foods ferment more readily in the gut and can increase gas production, particularly in sensitive individuals. Common culprits include beans, lentils, chickpeas, onions, garlic, cabbage, and cruciferous vegetables. High-FODMAP fruits and sugar alcohols found in processed foods may also trigger bloating. Functional Medicine recommends identifying personal triggers through an elimination and reintroduction approach rather than avoiding all potentially gassy foods indiscriminately.
3. What simple habits can help prevent trapped gas?
Eating slowly, chewing well, staying hydrated, and sitting up straight during meals support smoother digestion. Light movement, such as a short walk after meals, and relaxation practices to reduce stress, can also help your stomach feel lighter.
4. Can stress make gas worse?
Yes, stress can slow digestion and make bloating or trapped gas more noticeable. Mindful breathing, short relaxation exercises, or gentle stretching can help calm the digestive system naturally.
5. How can I tell if my gas is more than usual?
Occasional bloating is normal, but if fullness, pressure, or discomfort keeps returning, it may be linked to certain foods, habits, or gut sensitivities. Keeping a simple note of meals and how your stomach feels can help you notice patterns.
6. How does gut motility affect gas formation?
Slow gut motility prolongs the time food spends in the digestive tract, giving bacteria more opportunity to ferment undigested carbohydrates. Functional Medicine emphasizes supporting natural motility through movement, proper hydration, and adequate nutrient intake (such as magnesium), rather than relying on frequent small meals, which can disrupt the Migrating Motor Complex (MMC)—the gut’s natural cleansing mechanism that prevents bacterial overgrowth.
7. When should I seek professional advice?
If gas comes with persistent bloating, strong stomach discomfort, sudden weight changes, or digestive upset that doesn’t ease, it’s helpful to check in with a healthcare professional. Tracking symptoms makes it easier for them to provide personalized guidance
8. Can enzyme supplements or stomach acid support help reduce gas?
Yes, supporting digestive efficiency can reduce the substrate available for fermentation. Digestive enzymes, adequate stomach acid (when safely supported), and bile production help break down carbohydrates, fats, and proteins effectively. This reduces undigested food reaching the colon, limiting excessive bacterial fermentation and gas formation. Such strategies should be tailored to the individual under professional guidance.
9. How can Hormone Reset help with gas and bloating?
Hormone Reset focuses on identifying root causes—like thyroid function, gut health, or food sensitivities—and creating a tailored plan to support digestive comfort and reduce bloating naturally.
10. Can hormones or thyroid issues influence gas and bloating
Yes, hormonal imbalances—including thyroid dysfunction—can slow gut motility and alter digestion, making gas and bloating more likely. Functional Medicine considers these systemic influences when addressing digestive discomfort. Optimizing thyroid function, sex hormone balance, and overall metabolic health can significantly improve motility, enzyme activity, and gut microbiome function, reducing chronic gas.
Conclusion
Yes, hormonal imbalances—including thyroid dysfunction—can slow gut motility and alter digestion, making gas and bloating more likely. Functional Medicine considers these systemic influences when addressing digestive discomfort. Optimizing thyroid function, sex hormone balance, and overall metabolic health can significantly improve motility, enzyme activity, and gut microbiome function, reducing chronic gas.
Learn more about supporting hormone and digestive balance with the Hormone Reset program.
References
- Intestinal Gas Production:
Comprehensive review of how gut microbes generate intestinal gas, including mechanisms and contributing factors – ScienceDirect, 2025 - Gut Microbiota Dysbiosis in FGIDs:
Insights into how microbial imbalance drives symptoms and pathophysiology in functional gastrointestinal disorders – PubMed Central, 2024 - SIBO & Methane-Related Fermentation:
Detailed discussion on methane production, bacterial/fungal roles, diagnostic methods, and treatment strategies for SIBO – MDPI, 2023 - Small Intestinal Bacterial Overgrowth (SIBO):
Clinical overview of causes, symptoms, diagnostic criteria, and therapeutic approaches to SIBO – PubMed Central, 2024 - Excessive Gas:
Overview of causes, symptoms, and general guidance on managing gas –Mayo Clinic, 2025 - Tips for Healthy Digestion:
Practical strategies to support smooth digestion and reduce bloating –Harvard Health Publishing, 2024 - Digestive Health and Gas:
Insights into normal gas formation and digestive system function –National Institutes of Health (NIH), 2021 - Managing Gas and Bloating:
Professional guidance on recognizing and alleviating gas-related discomfort –American Gastroenterological Association, 2023 - Causes and Remedies for Gas
Evidence-based advice on foods, lifestyle habits, and natural relief methods –ClevelandClinic, 2023
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset