Autoimmune disorders are intricate conditions where the immune system mistakenly sees the body’s own tissues as invaders and attacks them. Take Hashimoto’s thyroiditis, for instance, it causes the immune system to harm the thyroid gland, which can lead to hypothyroidism.
On the flip side, Graves’ disease causes the thyroid to become overactive, leading to hyperthyroidism. These conditions don’t exist in isolation; they often show up alongside other autoimmune disorders like Type 1 diabetes, lupus, or rheumatoid arthritis. Grasping these connections is really important for effective treatment and support.
How Autoimmune Disorders Are Interconnected
Autoimmune illnesses tend to have certain shared risk factors that cause individuals problems, including genetics, environmental stimuli, and hormonal irregularities. As an example, an individual suffering from celiac disease may be experiencing Hashimoto’s as well, as such illnesses tend to be linked with each other in terms of related pathways of immune dysregulation.
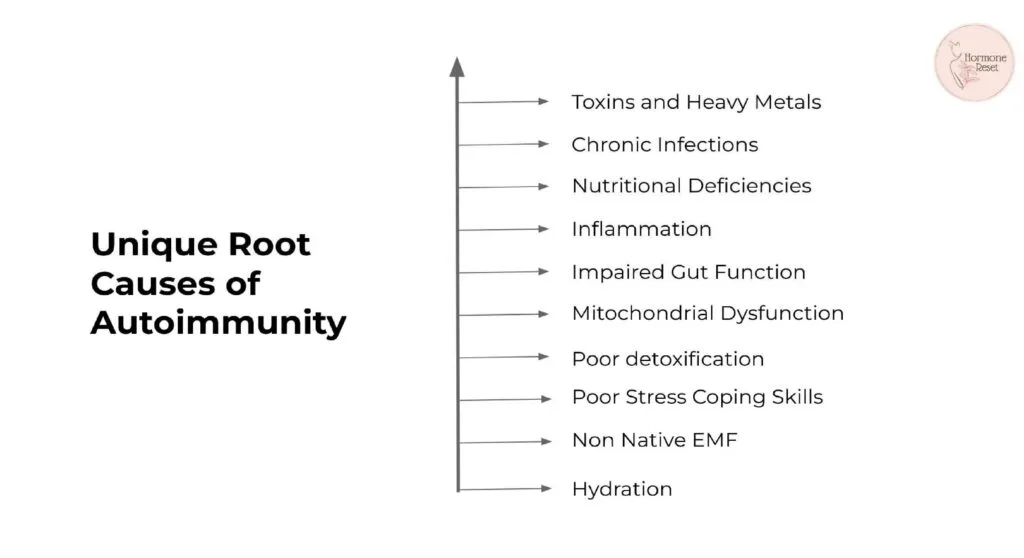
Environmental toxins, chronic infections, and gastrointestinal problems etc. may serve as catalysts, which initiate a chain reaction that results in different autoimmune diseases. This interdependence elegantly highlights the importance of holistic treatment.
The Role of Hormones in Autoimmune Diseases
Hormones are also important in controlling our immune system, and when they’re imbalanced, it can cause Interconnectedness of Autoimmune Disorders. Consider estrogen, for example; it’s incredible in how it aids immune function, but excessive amounts of it can actually make women more susceptible to autoimmune diseases. Likewise, chronic stress can cause cortisol levels to become elevated, which can interfere with immune tolerance and increase inflammation. And then there are our thyroid hormones, which are crucial to metabolism and tend to get affected in autoimmune diseases and cause a wide range of symptoms such as tiredness, weight fluctuations, and mood swings.
How hormonal imbalances impact specific autoimmune conditions:
- Dysregulated thyroid hormone function can shift immune tolerance and amplify inflammatory responses, further propelling autoimmunity.
- Hashimoto’s: Decreased thyroid hormones result in decreased metabolism and energy loss.
- Grave’s Disease: Increased thyroid hormones result in increased heart rate, anxiety, and weight loss.
- Lupus: Endocrine changes may precipitate flares, particularly during pregnancy or menopause.
- Insulin: Insulin resistance and long-term blood sugar disturbances may initiate systemic inflammation and immune dysregulation, predisposing to autoimmune conditions such as type 1 diabetes and rheumatoid arthritis.
- Estrogen: Estrogen potentiates immune reactions by promoting the production of B cells and pro-inflammatory cytokines, with a possible outcome of increased immune activity. This is why lupus, rheumatoid arthritis (RA), and multiple sclerosis (MS) are more prevalent in women
- Melatonin: Melatonin, being responsible for regulating sleep, is also immune-modulating. It decreases oxidative stress, modulates inflammatory cytokines, and maintains immune homeostasis. Low levels of melatonin and sleep disturbances are associated with enhanced autoimmune activity.
The Gut-Immune System Connection

Our gut is actually a key to maintaining our immune system! Occasionally, there’s an issue called leaky gut where the lining of the intestines becomes a bit too permeable. This can cause toxins and bits of food that haven’t been digested etc. to pass through into the bloodstream, and this makes our immune system go into overdrive. Unfortunately, this can then make most autoimmune diseases, such as Hashimoto’s and rheumatoid arthritis, even harder to control.
Ways to Restore Gut Health:
- Adding probiotics and prebiotics.
- After an anti-inflammatory diet of whole foods.
- Avoiding common triggers like gluten, dairy, and processed foods.
- With the use of target herbs and supplements such as aloe vera gel, marshmallow, vitamins A and D, Omega 3 fatty acids, zinc carnosine, etc. for the support of gut healing and repair.
Environmental Triggers and Interconnectedness of Autoimmune Disorders
There are certain toxins such as heavy metals, pesticides, and endocrine disruptors, which have a significant Environmental Triggers Influence Autoimmune Conditions. These toxins tend to alter our immune system’s function, destabilize our hormones, and contribute to increased inflammation.
Steps to Minimize Environmental Toxins:
- Use natural personal care and cleaning products.
- Consume organic, non-gmo, pesticide-free food. Avoid processed food.
- Filter drinking water to minimize exposure to heavy metals.
- Enhance indoor air quality
- Be cautious while using plastic products. Reduce plastics, particularly when coming into contact with liquid food products.
- Keep detox channels open and follow regular detox regimen.
- Make yourself aware of sources of heavy metals such as mercury, aluminium, lead etc. and avoid them.
Also Read: Living with Multiple Autoimmune Conditions
Why Conventional Treatments Fall Short?
When dealing with autoimmune disorders, most conventional therapies will focus on symptom control rather than actually addressing the root causes. Consider Hashimoto’s, for instance; while thyroid hormone replacement may be a typical treatment, it doesn’t really stop the immune system’s assault on the gland.
In the same way, for Graves’ disease, treatments such as anti-thyroid drugs or surgery can be used, but they can at times cause complications in the future. Moreover, they tend to overlook treating key aspects such as gut health, inflammation, or environmental toxin exposure, which initially triggered the autoimmunity. This traditional method leaves patients vulnerable to future symptoms and even the onset of new autoimmune conditions.
How Lifestyle Changes Can Reduce Autoimmune Risk
Lifestyle factors such as diet, exercise, and stress management can significantly impact autoimmune disease outcomes. Adopting a healthier lifestyle can reduce inflammation, balance hormones, and improve overall immune function.
Key Lifestyle Adjustments:
- Exercise: Regular Exercise regulate immune function and reduce inflammation.
- Stress reduction: practices like meditation and yoga lower cortisol levels.
- Sleep Hygiene: Adequate sleep supports hormone regulation and immune repair.
- Diet: Organic, whole, unprossesed
How can we Heal Autoimmune Disorders?

In the case of autoimmune diseases, accepting a holistic and individualized way of dealing with them makes all the difference! Protocols like Hormone Reset seek to discover the underlying causes of these diseases, making you feel better rather than simply alleviating the symptoms.
Key Features of a Comprehensive Healing Approach:
Personalized Nutrition:
It’s great to emphasize adding anti-inflammatory foods to our diet, like colorful leafy greens, tasty wild-caught fish, and nutritious nuts that can calm the immune system. Avoiding common culprits like gluten, dairy, and processed foods at the same time can make a big difference, as these tend to exacerbate autoimmune responses.
Gut Health Restoration:
It will help to mend leaky gut, a syndrome where toxins and food particles do not get eliminated by digestion but rather enter into the bloodstream to stimulate immune responses. Using prebiotics, probiotics, and healing foods such as bone broth can be great methods for healing and securing the gut lining.
Stress Reduction:
This brings in some wonderful stress management methods that can make a real difference! Delight in the soothing processes of yoga, deep breathing, and mindfulness, all of which are wonderful for reducing cortisol levels. It’s also a gentle reminder of just how important it is to cultivate regular sleep habits since these help to reset your body’s stress levels and encourage a more tranquil and balanced life response.
Detoxification:
This methodology focuses on the necessity to eliminate environmental pollutants, heavy metals, and other toxins that harm immune function. It also identifies the use of natural detoxifying foods, such as healthy cruciferous vegetables and adequate hydration, to provide protection for the liver and general health kidneys.
Hormone Balancing:
This strategy combines natural supplements, like adaptogens, with careful lifestyle modifications to keep hormonal ups and downs in check. It’s all about tailoring interventions to suit individual requirements, addressing certain imbalances carefully in thyroid, cortisol, and sex hormones.
The Future of Autoimmune Care
Autoimmune diseases certainly thrive on a holistic and individualized protocol! Protocols such as Hormone Reset target the origins of autoimmune diseases by encouraging hormone balance, facilitating a healthy gut, minimizing stress, and fostering detoxification. This multifaceted strategy not only provides symptom relief but aims to discourage the worsening and clustering of autoimmune diseases.
If you’re excited to take charge of your health and heal from the inside out, a functional medicine approach provides a wonderful pathway to long-term wellness. Now is the perfect time to restore balance and reclaim your vibrant energy!
References
- Brent GA. Environmental exposures and autoimmune thyroid disease. Thyroid. 2010;20:755–61
- Ferrari SM, Fallahi P, Ruffilli I, Elia G, Ragusa F, Benvenga S, Antonelli A. The association of other autoimmune diseases in patients with Graves’ disease (with or without ophthalmopathy): Review of the literature and report of a large series. Autoimmun Rev. 2019 Mar;18(3):287-292.
- Franco JS, Amaya-Amaya J, Anaya JM. Thyroid disease and autoimmune diseases. In: Anaya JM, Shoenfeld Y, Rojas-Villarraga A, et al., editors. Autoimmunity: From Bench to Bedside [Internet]. Bogota (Colombia): El Rosario University Press; 2013 Jul 18. Chapter 30.
- Kaur J, Jialal I. Hashimoto Thyroiditis. [Updated 2025 Feb 9]. In: StatPearls [Internet]. Treasure Island (FL):
Share