Table of Contents
Weight loss is one of the most misunderstood aspects of modern health. Millions of people eat “right” and exercise “enough,” only to wonder why the scale doesn’t move — or worse, why belly fat and inflammation continue to worsen. This frustration is real, and it often stems not from lack of effort but from systems within the body that have not been addressed. In functional medicine, weight loss isn’t just about calories — it’s about the internal environment that determines how your metabolism behaves.
In this long‑form article, we’ll explore why traditional approaches often fail, and how the gut, hormones, and liver are central to sustainable fat loss. We’ll look at current science, functional medicine concepts, and practical root‑cause frameworks — all grounded in the latest understanding of metabolic regulation.
The Calorie Myth: Why Simple Math Doesn’t Match Biology
For decades, weight loss has been explained as “calories in vs. calories out.” While this model sounds logical, it fails to capture the complex biochemical and hormonal feedback loops that govern energy homeostasis.
Your body is not a machine. It is a biological ecosystem designed to maintain stability (homeostasis). When systems like hormone signaling, gut integrity, or liver function are disrupted, the body adapts in ways that protect energy stores rather than melt them away.
For example:
- The brain constantly monitors energy availability. When it senses stress, inflammation, or nutrient deficiencies, it signals the body to store fat as insurance.
- Chronic stress and elevated cortisol drive glucose dysregulation and fat storage, even without overeating.
- Disruptions in gut microbiota can alter the production of signaling molecules that regulate appetite, metabolism, and insulin sensitivity.
This science helps explain why many people can eat less and still gain weight, or why “starving yourself” can paradoxically slow metabolism.
The Hormone Connection: Metabolic Regulators That Control Fat Storage
Hormones are the chemical messengers that orchestrate metabolism. When they are imbalanced, fat loss resistance is one of the most common outcomes.
Insulin: The Master Fat Storage Hormone
Insulin regulates glucose uptake and storage. When insulin is constantly elevated — due to high refined carbohydrate intake, frequent snacking, or chronic stress — the body shifts into a fat storage mode. This state is often called insulin resistance, and it is a common early step on the path to metabolic dysfunction.
Research increasingly shows that imbalances in insulin and related pathways contribute to both obesity and metabolic syndrome.
Cortisol: The Stress Hormone That Stores Fat
Cortisol is released in response to stress. Short‑term elevations are adaptive, but chronic cortisol elevation:
- Increases appetite
- Promotes visceral fat storage
- Suppresses thyroid function
- Drives blood sugar variability
Chronic cortisol elevation can therefore create a metabolic environment that favors weight gain — especially around the abdomen.
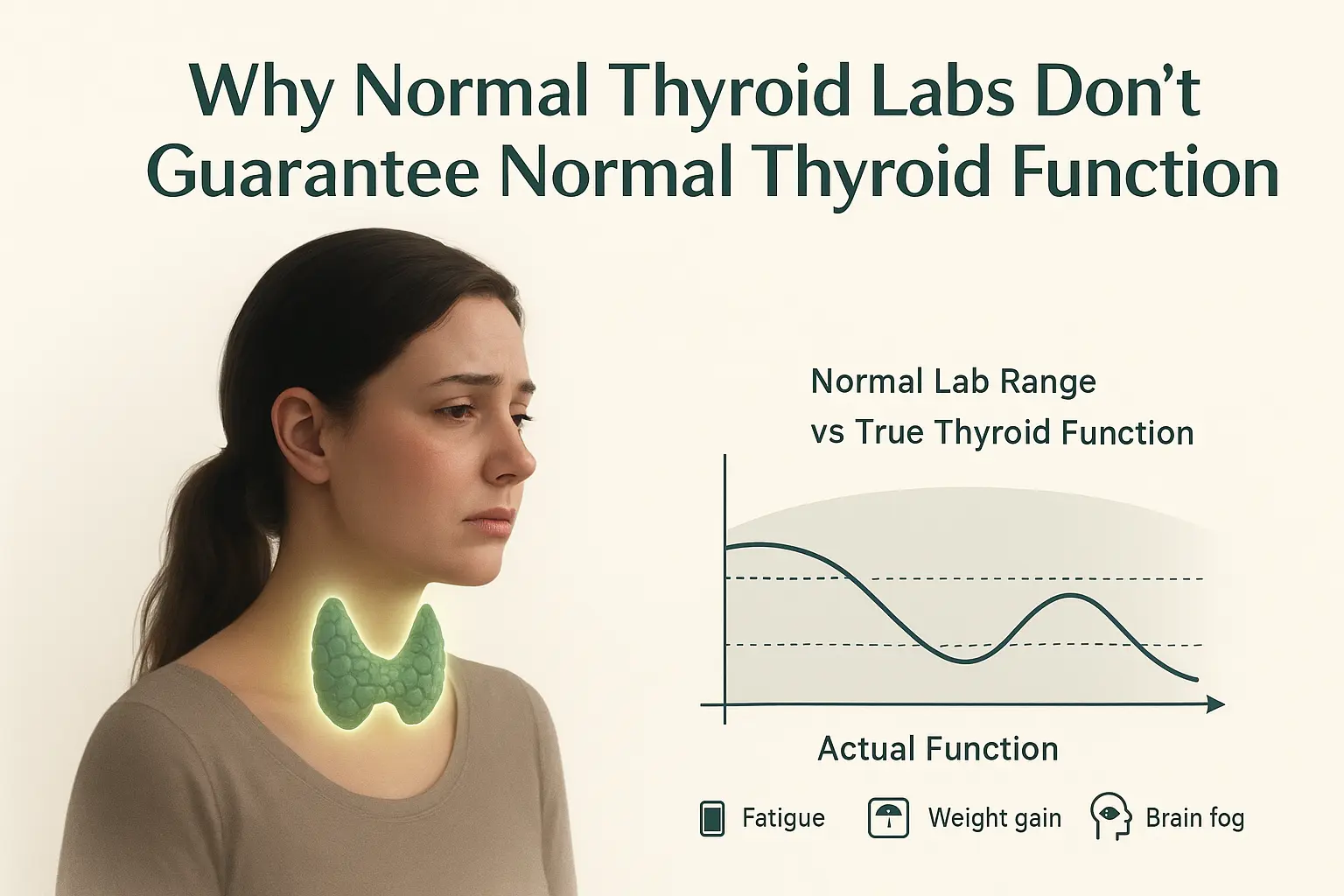
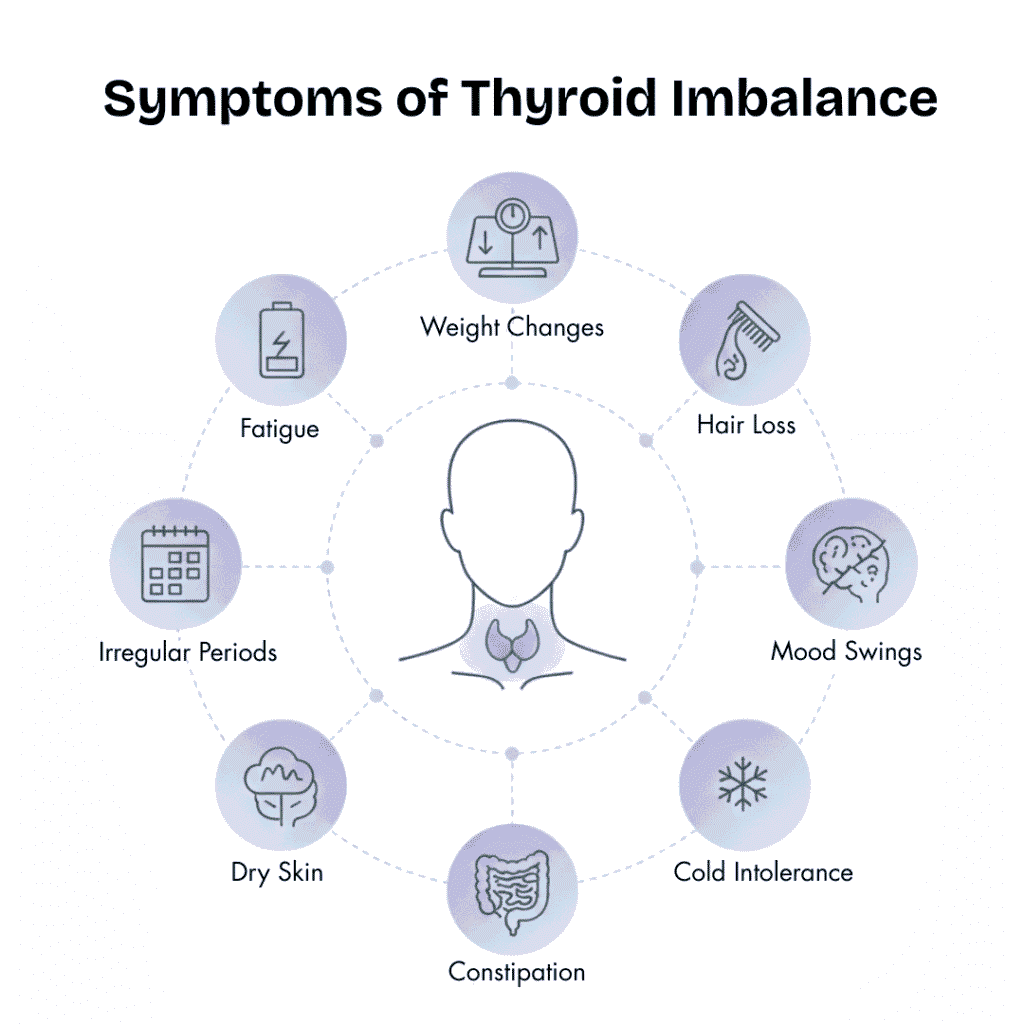
Thyroid Hormones: The Metabolic Accelerator
Thyroid hormones (T3 and T4) influence every cell’s metabolism. When thyroid function is suboptimal — even within “normal” lab ranges — metabolic rate drops, energy levels decline, and weight becomes more difficult to lose.
Functional medicine practitioners often look beyond standard TSH tests to evaluate:
- Free T3 and Free T4
- Reverse T3 (an inactive form that blocks metabolism)
- Thyroid antibodies
Because thyroid activity influences nearly every aspect of energy regulation, even mild dysfunction can be a key root cause of weight resistance.
Sex Hormones: Estrogen, Progesterone & Testosterone
Sex hormones also shape metabolic outcomes:
- Estrogen dominance is linked with increased fat storage and reduced fat burning
- Low progesterone can impact insulin sensitivity and inflammation
- Low testosterone (in both men and women) reduces lean mass and slows metabolism
Functional pathways that connect hormone imbalances with metabolic resistance are deeply interconnected with liver processing and gut microbial function.
The Gut’s Role in Metabolism: More Than Digestion
The gut microbiome is now understood as an endocrine organ — producing signaling molecules that influence metabolism, inflammation, appetite, and fat storage.
Gut Microbiota as Metabolic Regulators
Dysbiosis — an imbalance in gut microbes — has been linked to:
- Increased inflammation
- Reduced production of short‑chain fatty acids (SCFAs) that support metabolic health
- Greater gut permeability (“leaky gut”)
- Altered appetite signaling through gut‑brain peptides
These microbial and biochemical changes can increase fat storage, drive insulin resistance, and make weight loss challenging even with diet and exercise.
A comprehensive review highlights the impact of the microbiome on obesity and metabolic disorders, showing that gut microbial shifts can directly influence:
- Appetite
- Lipid metabolism
- Immune activation
- Energy homeostasis SpringerLink
Gut‑Brain Axis & Metabolism
The gut and brain communicate via hormonal and neural pathways that regulate hunger and satiety. When this axis is dysregulated — due to poor gut health or chronic inflammation — the signals that tell you “you’re full” or “you have enough energy” are blurred. This contributes to overeating, cravings, and poor metabolic control.
Functional Medicine Viewpoint
Rather than treating the gut as a passive digestive organ, functional medicine sees it as central to:
- Hormone balance
- Immune function
- Detoxification support
- Neuroendocrine signaling
Thus, poor gut health can be a root cause of metabolic resistance.
The Liver: The Metabolic Control Center
In functional medicine, the liver is recognized as the body’s primary metabolic hub, coordinating nutrient processing, hormone regulation, detoxification, and fat metabolism. While the gut handles intake, the liver ensures that nutrients are efficiently utilized, hormones are cleared, toxins neutralized, and fats are properly digested through bile production. It also plays a critical role in regulating blood sugar and maintaining metabolic flexibility.
Compromised liver function—due to fat accumulation, chronic inflammation, or exposure to environmental toxins—is increasingly seen as a barrier to sustainable weight loss, both in India and globally. Subclinical liver stress often goes undetected, yet it impairs metabolism by disrupting hormone clearance, nutrient processing, and energy homeostasis.
Fatty Liver and Insulin Resistance: Non-alcoholic fatty liver disease (NAFLD) is a common metabolic condition associated with obesity, insulin resistance, and systemic inflammation. A fatty liver struggles to regulate blood glucose, produces pro-inflammatory cytokines, and sends stress signals to other organs, further impairing metabolic efficiency. (Journal of Clinical Endocrinology & Metabolism, 2021)
Functional medicine interventions for liver health include:
- Anti-inflammatory and nutrient-dense diet to reduce fat accumulation and oxidative stress.
- Supporting detox pathways with nutrients like N-acetylcysteine, milk thistle, B vitamins, and antioxidants.
- Managing blood sugar and insulin through diet, lifestyle, and gut health optimization.
- Reducing environmental toxin exposure and chronic alcohol or medication stressors.
Outcome: By restoring liver function, metabolic signaling improves, hormone clearance normalizes, inflammation decreases, and fat-burning capacity is enhanced. Functional medicine treats liver health as a cornerstone of systemic metabolic restoration, ensuring that weight loss is sustainable and rooted in overall wellness.
Chronic Inflammation: The Hidden Barrier to Weight Loss
Chronic inflammation is like a silent brake on your metabolism. Unlike short-term inflammation that helps your body heal, long-lasting inflammation disrupts hormones, blood sugar control, and energy use, making it hard to lose weight.
What Causes Chronic Inflammation?
- Leaky Gut: When the gut lining is weak, food particles, bacteria, and toxins leak into the bloodstream, triggering the immune system.
- Toxins: Pollution, heavy metals, and chemical exposures increase stress in the body and trigger inflammatory responses.
- Stress: Constant psychological or physical stress raises cortisol, promoting belly fat and insulin resistance.
- Gut Imbalance or Hidden Infections: Overgrowth of harmful gut bacteria or low-level infections keep the immune system activated.
How Inflammation Blocks Fat Loss:
- Insulin Resistance: Inflammatory molecules make it harder for cells to use sugar properly, encouraging fat storage.
- Appetite Hormone Disruption: Leptin and ghrelin signals get confused, making you feel hungrier and less satisfied after meals.
- Energy Conservation Signals: Cells slow down metabolism because they perceive stress, preventing fat burning.
- Reduced Flexibility: Your body struggles to switch between burning sugar and fat efficiently.
Functional Medicine Approach:
Functional medicine focuses on finding and fixing the root cause. Healing the gut, reducing toxins, balancing microbes, improving diet, supporting the liver, and managing stress can calm inflammation. Once inflammation is lowered, hormones stabilize, metabolism improves, and weight loss becomes easier and sustainable.
Stress, Sleep & Metabolism: Why the Nervous System Matters
Chronic stress is not just mental — it has physiological metabolic consequences. Elevated stress and poor sleep disrupt:
- Cortisol rhythms
- Appetite hormones
- Blood sugar control
- Mitochondrial function (how cells burn fuel)
These effects make fat loss harder, even with disciplined eating and activity.
Nutrient Deficiencies and Metabolic Blockage: A Functional Medicine Perspective
In functional medicine, nutrient sufficiency is foundational to metabolism, hormone function, and overall health. Micronutrients are not optional—they act as co-factors for enzyme activity, hormone synthesis, neurotransmitter balance, and detoxification pathways. Deficiencies can silently create metabolic resistance, making weight loss extremely difficult despite diet and exercise.
Vitamin D: Crucial for immune modulation, insulin sensitivity, and thyroid regulation. Low vitamin D is strongly associated with metabolic syndrome, obesity, and increased inflammatory markers. Supplementation under supervision can improve insulin signaling and hormone balance.
Magnesium: Required for over 300 enzymatic reactions, including those controlling energy production and glucose metabolism. Magnesium deficiency is linked to insulin resistance, poor energy utilization, and impaired mitochondrial function.
B Vitamins: B12, B6, and folate are essential for methylation, neurotransmitter production, and homocysteine regulation. Deficiency can lead to fatigue, impaired thyroid function, and disrupted hormone metabolism.
Zinc: Integral to thyroid hormone synthesis, insulin regulation, and appetite signaling. Zinc deficiency can increase oxidative stress, hormonal imbalance, and metabolic inefficiency.
Other Micronutrients: Selenium, iron, omega-3 fatty acids, and antioxidants support liver detoxification, hormone clearance, and inflammatory balance, all of which are critical for fat metabolism.
Functional medicine practitioners often use detailed lab testing to identify deficiencies and tailor supplementation, while also addressing underlying causes such as gut malabsorption, chronic inflammation, or toxin exposure. Correcting these deficiencies is not simply about filling gaps—it unlocks metabolic pathways, improves hormonal function, and restores energy regulation, paving the way for sustainable, root-cause weight management.
Functional Assessment: How Practitioners Identify Root Causes
Functional medicine views the body as an interconnected system, where metabolic, hormonal, immune, and digestive pathways constantly interact. Unlike conventional approaches that focus primarily on weight, BMI, or isolated lab values, functional medicine practitioners use comprehensive assessments to uncover root causes of metabolic resistance and fat accumulation.
Hormone Panels: Detailed evaluation of thyroid (TSH, Free T3, Free T4, Reverse T3, thyroid antibodies), adrenal hormones (cortisol rhythm), sex hormones (estrogen, progesterone, testosterone), and appetite-regulating hormones (leptin, ghrelin) helps identify imbalances that influence energy expenditure, fat storage, and cravings.
Blood Sugar and Insulin Response: Functional medicine tests often include fasting glucose, HbA1c, fasting insulin, and oral glucose tolerance to detect insulin resistance, a key driver of metabolic dysregulation and fat accumulation.
Gut Microbiome Analysis: Dysbiosis and leaky gut contribute to systemic inflammation, hormone disruption, and altered nutrient absorption. Stool tests, microbiome sequencing, and evaluation of gut permeability markers guide interventions.
Nutrient Status: Deficiencies in vitamin D, magnesium, B vitamins, zinc, and omega-3s are assessed as these are critical co-factors in hormone production, mitochondrial function, and detoxification.
Liver Detox Capacity and Inflammatory Markers: Liver function tests, CRP, IL-6, and other markers indicate metabolic stress and systemic inflammation, both of which impair fat loss.
Stress and Nervous System Evaluation: Cortisol rhythms, heart rate variability, and lifestyle stressors are assessed to understand their impact on hormone signaling and metabolic flexibility.
By examining these systems holistically, functional medicine practitioners identify the interconnected patterns that block weight loss and develop personalized, root-cause strategies rather than offering generic solutions.
Lifestyle Factors That Block Weight Loss: A Functional Medicine Perspective
Weight loss resistance is rarely caused by a single factor. Modern lifestyles create multiple stressors that disrupt metabolism, hormone balance, and gut-liver function, often invisibly.
1. Sedentary Behaviour: Prolonged sitting and low physical activity reduce mitochondrial efficiency, impair insulin sensitivity, and slow fat oxidation. Research shows even moderate activity, such as short bouts of walking or strength training, improves glucose metabolism and hormone regulation.
2. Highly Processed Diets: Diets rich in refined carbohydrates, trans fats, and ultra-processed foods promote chronic inflammation, dysbiosis, and insulin resistance. Functional medicine emphasizes nutrient-dense, anti-inflammatory foods to restore gut microbiome balance, support liver detoxification, and stabilize hormones.
3. Irregular Sleep: Poor or inconsistent sleep impairs cortisol rhythms, disrupts leptin and ghrelin signaling (hunger hormones), and reduces energy expenditure. Chronic sleep deprivation is linked to increased visceral fat and impaired metabolic flexibility.
4. Chronic Stress: Persistent psychological or physical stress elevates cortisol, which drives abdominal fat accumulation, insulin resistance, and thyroid suppression. Stress also worsens gut permeability, further amplifying inflammation and metabolic disruption.
5. Environmental Toxins: Exposure to endocrine-disrupting chemicals (EDCs) such as BPA, pesticides, and heavy metals can interfere with thyroid function, liver detoxification, and hormone signaling, all critical for weight regulation.
Functional medicine recognizes that these lifestyle factors interact with gut, liver, and hormone systems, creating a vicious cycle that prevents fat loss. Addressing these root contributors—through diet, sleep, stress management, detox support, and movement—restores metabolic balance and enables sustainable weight loss.
Functional Medicine Strategies That Support Metabolic Healing & Weight Loss
Functional medicine approaches weight loss as a natural outcome of restoring internal systems, rather than focusing solely on calories or exercise. Sustainable results depend on addressing the gut, hormones, liver, inflammation, and stress — the key drivers of metabolic health.
1. Gut Repair: The gut is a central regulator of metabolism and immune signaling. Dysbiosis, leaky gut, or microbial imbalances can trigger systemic inflammation, impair appetite regulation, and block fat burning. Functional medicine interventions include probiotics, prebiotics, gut-healing nutrients (like L-glutamine and zinc), and anti-inflammatory diets.
2. Hormone Balancing: Hormones orchestrate fat storage and energy use. Imbalances in thyroid, insulin, cortisol, estrogen, progesterone, and leptin can create resistance to weight loss. Personalized strategies focus on optimizing hormone levels, improving insulin sensitivity, and regulating stress hormones.
3. Liver Support: The liver processes nutrients, detoxifies hormones, and regulates metabolism. Impaired liver function from toxins or fatty liver slows fat metabolism. Functional medicine emphasizes detox support, nutrient cofactors, and reducing environmental and dietary toxins.
4. Inflammation Reduction: Chronic inflammation disrupts insulin signaling, appetite hormones, and metabolism. Strategies include anti-inflammatory diets, micronutrient support (vitamin D, magnesium, zinc), and addressing underlying triggers such as gut permeability and environmental toxins.
5. Stress & Sleep Optimization: Chronic stress elevates cortisol, while poor sleep impairs insulin sensitivity and metabolic regulation. Functional medicine incorporates stress management, meditation, sleep hygiene, and adaptogens to restore balance.
6. Personalized Root-Cause Approach: Every individual’s metabolic resistance is unique. Functional medicine combines comprehensive testing, dietary, lifestyle, and behavioral interventions to target the root causes, ensuring fat loss occurs naturally as internal systems normalize.
Outcome: By healing the gut, balancing hormones, supporting the liver, reducing inflammation, and managing stress, the body can reset its metabolism, allowing sustainable, long-term weight loss as a byproduct of restored health.
Why Results May Take Time and Require Personalization?
Functional medicine works on the principle that every body is unique, and weight loss or metabolic restoration cannot be achieved with a single quick fix. Long-term results depend on identifying and correcting the underlying factors that block metabolism.
Why it Takes Time:
- Multiple Systems Are Involved: Weight resistance is rarely due to one issue. Gut health, liver function, hormones, inflammation, sleep, and stress all interact. Addressing just one factor may provide temporary relief but not lasting results.
- Complex Biological Patterns: Each individual has a distinct combination of hormone imbalances, nutrient deficiencies, and environmental exposures that affect metabolism differently. Functional medicine maps these patterns before making targeted interventions.
- Healing and Adaptation: Restoring gut integrity, balancing hormones, improving liver detoxification, and reducing inflammation takes time. Cells, tissues, and metabolic pathways need weeks or months to recover and function efficiently.
- Building Sustainable Habits: Functional medicine emphasizes long-term lifestyle changes in diet, movement, sleep, and stress management. Quick fixes may yield temporary results but often fail when old habits resume.
Why Conventional Approaches Often Fall Short:
Traditional methods frequently focus on calorie restriction or medication to suppress symptoms rather than addressing root causes. This may produce short-term results, but underlying imbalances remain, leading to plateaus, fatigue, and frustration.
By tackling the body’s systems holistically and allowing time for true healing, functional medicine enables lasting metabolic balance, hormone stability, and gradual, sustainable weight loss.
FAQs: Functional Medicine & Weight Loss
1. Why am I eating healthy and exercising, yet not losing weight?
Weight loss resistance often stems from internal system imbalances rather than calorie intake alone. Hormonal disruption (thyroid, insulin, cortisol), gut dysbiosis, liver stress, chronic inflammation, and nutrient deficiencies can all signal your body to store fat, making conventional diet and exercise less effective.
2. How does gut health affect my metabolism?
The gut microbiome produces hormones and signaling molecules that regulate appetite, fat storage, and insulin sensitivity. Dysbiosis (microbial imbalance) or leaky gut increases inflammation, disrupts metabolism, and alters hunger cues, contributing to weight gain or stalled weight loss.
3. What role does the liver play in fat loss?
The liver is central to metabolic control: it processes nutrients, detoxifies hormones, regulates blood sugar, and produces bile for fat digestion. Fatty liver, toxin accumulation, or chronic inflammation can impair these functions, slowing metabolism and fat-burning capacity.
4. How do hormones influence weight loss?
Hormones such as insulin, cortisol, thyroid hormones, estrogen, progesterone, and leptin orchestrate energy use and fat storage. Imbalances—like insulin resistance, thyroid sluggishness, or estrogen dominance—can block fat loss, even with proper diet and exercise.
5. Why is chronic inflammation a problem for weight loss?
Persistent inflammation alters insulin and appetite hormone signaling, signals cells to store energy, and reduces metabolic flexibility. Sources include gut permeability, environmental toxins, stress, and hidden infections.
6. Can nutrient deficiencies prevent weight loss?
Yes. Micronutrients like vitamin D, magnesium, B vitamins, zinc, selenium, and omega-3 fatty acids are critical co-factors for hormone production, enzyme function, and detox pathways. Deficiencies can impair metabolism, energy production, and fat-burning efficiency.
7. How long does it take to see results using functional medicine principles?
Because functional medicine addresses multiple systems simultaneously, improvements may take weeks to months. The focus is on restoring internal balance—gut, hormones, liver, and inflammation—which gradually leads to sustainable fat loss.
Conclusion: Metabolic Healing Before Weight Loss
Weight loss is not just about eating less and moving more. It’s about understanding the internal signals that determine whether your body releases or stores fat.
Further research increasingly supports the idea that gut microbiota influences metabolic homeostasis, that hormonal imbalances can drive fat storage, and that liver function is essential for energy balance
Functional medicine reframes weight loss as a signal of internal balance rather than a battle against your body. When hormones communicate clearly, when the gut and liver function optimally, and when inflammation is controlled, fat loss becomes a natural consequence of restored health.
Book Your Functional Medicine Consultation Today – Heal your metabolism, balance hormones, and achieve lasting results.

References
- Impact of the gut microbiota on inflammation, obesity, and metabolic disease -Springer Nature
- Insights into the role of gut microbiota in obesity: pathogenesis & therapeutic perspectives– Oxford Academic
- Gut Microbiota as a Trigger for Metabolic Inflammation in Obesity and Type 2 Diabetes-National Library of Medicine
- Exploring the Gut Microbiota: Key Insights Into Its Role in Obesity, Metabolic Syndrome, and Type 2 Diabetes – The Journal of Clinical Endocrinology & Metabolism
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset