Table of Contents
Brain fog and depression often develop gradually. Concentration becomes harder, mental stamina declines, and motivation feels inconsistent. Many people attribute these changes to stress, workload, or aging. Others assume the problem is purely psychological. In reality, cognitive and emotional symptoms frequently reflect underlying physiological imbalance rather than a lack of effort or resilience.
Functional medicine approaches brain fog and depression by examining how systems within the body interact. Instead of focusing only on symptom categories, it evaluates hormonal signaling, metabolic stability, inflammation, and stress response patterns that influence brain function over time.

Why Brain Fog and Depression Commonly Appear Together?
Brain fog and depression share overlapping biological pathways. Both are influenced by chronic stress, inflammatory signaling, sleep disruption, and energy regulation at the cellular level. When these systems are strained, the brain prioritizes survival functions over higher cognitive processing.
This shift can reduce mental clarity, slow information processing, and limit emotional adaptability. From a functional medicine perspective, these symptoms indicate that the nervous system is under sustained load rather than failing to perform correctly.
How does the Functional Medicine Approach to Mental Health?
Functional medicine views mental health as inseparable from overall physiology. The brain depends on consistent hormonal input, stable blood glucose, adequate nutrient availability, and regulated immune activity. Chronic inflammation also has a disproportionate impact on the brain. When one or more of these factors become dysregulated, cognitive and emotional symptoms may emerge.
Rather than treating brain fog or depression as isolated conditions, functional medicine evaluates patterns across systems. This includes assessing stress response, hormonal rhythms, evaluating the gut-brain axis, including digestive function, and metabolic balance. The objective is to understand why the brain is receiving signals that impair focus, mood, and mental endurance.
The Vagus Nerve and Nervous System Regulation
The vagus nerve acts as a primary communication pathway between the brain, gut, and immune system, influencing stress recovery, inflammation, and emotional regulation. Reduced vagal tone is associated with diminished nervous system flexibility, which may contribute to brain fog, low mood, and poor stress tolerance.
Chronic stress, sleep disruption, and inflammatory load can weaken vagal signaling over time. Supporting nervous system regulation is, therefore, a key component of restoring cognitive clarity and emotional resilience.
The Influence of Hormones on Mood and Cognitive Function
Hormones act as signaling molecules that regulate how the brain processes information, responds to stress, and maintains emotional stability. Disruptions in hormonal communication can significantly affect mental performance.
Stress Hormones and Cognitive Load
Cortisol supports alertness and energy mobilization during short-term stress. Prolonged stress exposure, however, can alter cortisol rhythms. This often results in mental fatigue, difficulty concentrating, heightened anxiety, or low motivation. The brain remains in a heightened state of vigilance while lacking the capacity for sustained focus.
Thyroid Hormones and Mental Processing
Thyroid hormones influence neuronal energy production. Stress reduces thyroid function. Suboptimal thyroid signaling may slow cognitive speed, impair memory, and reduce mental clarity. These effects are frequently subtle and may occur even when standard laboratory values appear within reference ranges.
Blood Sugar Regulation and Brain Stability
The brain requires a consistent energy supply. Fluctuating blood glucose levels, often caused by fluctuations in stress hormones, can contribute to irritability, attention difficulties, and mental fatigue. Repeated instability places additional stress on the nervous system and may worsen depressive symptoms over time.
Sex Hormones and Emotional Regulation
Estrogen, progesterone, and testosterone interact with neurotransmitter systems involved in mood and motivation. Hormonal shifts related to life stages, chronic stress, or metabolic changes can influence emotional resilience and cognitive performance.
The Gut–Brain Relationship in Brain Fog and Depression
The gastrointestinal system plays a role in immune regulation, neurotransmitter production, and hormone metabolism. When digestive function is compromised, inflammatory signaling may increase and interfere with normal brain activity.
Alterations in gut health can also affect how hormones are processed and eliminated, contributing to prolonged hormonal imbalance. Addressing digestive function is therefore a relevant component in managing persistent cognitive and mood-related symptoms.
Common Environmental Toxins That May Affect Brain Health
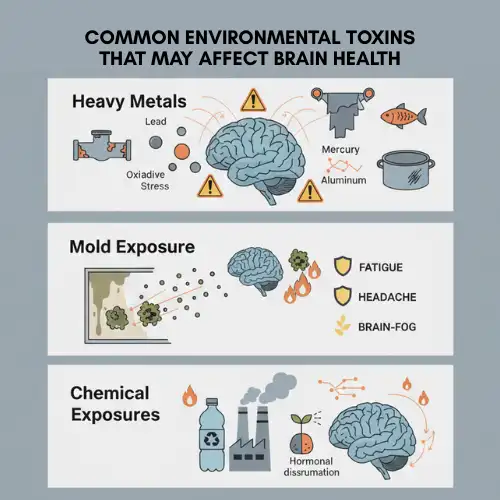
Heavy Metals
- Lead, mercury, cadmium, and aluminum can accumulate over time.
- Sources: old paint and plumbing, contaminated water, large fish, and some cookware.
- Effects: brain fog, memory issues, reduced concentration via oxidative stress and disrupted neuronal signaling.
Mold Exposure
- Occurs in water-damaged homes or workplaces.
- In some individuals, mold toxins trigger immune activation and inflammation.
- Symptoms: persistent brain fog, fatigue, headaches, mood changes, respiratory issues, and joint discomfort.
- Response depends on immune sensitivity, detoxification, and overall resilience.
Chemical Exposures
- Pesticides, plastics, cleaning products, and industrial pollutants can act as neurotoxic or endocrine-disrupting agents.
- Effects: increased inflammation, oxidative stress, and hormonal imbalance affecting brain function.
- Risk is higher with combined environmental or metabolic stressors.
Why Hormonal Imbalance Requires a Systems-Based Approach?
Hormonal regulation depends on coordination between multiple systems, including the nervous system, endocrine glands, liver, and gut. Isolated interventions often fail to produce lasting results if contributing factors remain unaddressed.
Some practitioners describe the process of restoring hormonal signaling as a Hormone Reset, meaning a structured effort to reduce physiological stressors and support regulatory balance. This term refers to gradual restoration rather than rapid intervention and emphasizes system-wide support instead of isolated correction.
Changes Commonly Observed When Regulation Improves
As hormonal and metabolic stability improves, individuals often report steadier concentration, improved emotional regulation, and more consistent energy levels. These changes typically occur progressively rather than suddenly.
Improved mental clarity reflects enhanced system regulation rather than suppression of symptoms. The nervous system becomes more adaptable and less reactive to everyday stressors.
Who May Benefit from a Functional Medicine Approach?
A functional medicine evaluation may be appropriate for individuals experiencing persistent brain fog, depression accompanied by fatigue, anxiety associated with chronic stress, or cognitive changes during hormonal transitions. It can also be useful when conventional approaches provide incomplete relief.
This model does not replace psychological or psychiatric care. Instead, it addresses physiological contributors that influence mental health outcomes.
Frequently Asked Questions (FAQs)
1. Can a hormonal imbalance cause brain fog and depression?
Hormonal imbalance can contribute to both brain fog and depressive symptoms. Hormones influence how the brain regulates energy, stress responses, and neurotransmitter activity. When hormonal signaling becomes disrupted—due to chronic stress, metabolic instability, or inflammation—cognitive clarity and emotional regulation may be affected.
2. How does functional medicine approach brain fog differently?
Functional medicine looks beyond symptoms and examines underlying physiological factors that influence brain function. This includes evaluating stress hormones, thyroid function, blood sugar regulation, gut health, and inflammatory patterns. The goal is to understand why brain fog is occurring rather than managing it in isolation.
3. Is brain fog always related to mental health conditions?
Brain fog is not always caused by psychological conditions. It can result from hormonal changes, metabolic issues, sleep disruption, nutrient deficiencies, toxicity, or chronic inflammation. In many cases, cognitive symptoms reflect systemic imbalance rather than a primary mental health disorder.
4. Can functional medicine be used alongside conventional mental health treatment?
Yes. Functional medicine is often used alongside psychological or psychiatric care. It does not replace conventional treatment but may help address physiological factors that influence mental health, potentially improving overall treatment outcomes.
Closing Perspective
Brain fog and depression are not solely psychological experiences. They often represent physiological responses to ongoing internal imbalance. When hormonal signaling, metabolic stability, and inflammatory regulation improve, cognitive and emotional function frequently improves as well.
Functional medicine emphasizes understanding these underlying relationships. By addressing contributing factors across systems, it supports long-term mental clarity and emotional stability without relying on short-term symptom management alone.
👉 Book a consultation to address the root cause and restore mental clarity today.

References
- Functional Medicine Approach to Brain Fog– Cutler Integrative Medicine
- Functional Medicine for Depression– Dr. David Wiss
- Functional Medicine For Brain Fog– Dr. Stavy
- Functional Medicine: A Whole-Person Approach– MindRx Group
- Brain Fog Explained: Causes, Symptoms & How to Clear Your Mind– Eskag Sanjeevani
- Can Functional Medicine Help with Anxiety—Without Medication?– Michigan Health & Wellness Center
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset