Table of Contents
Rheumatoid Arthritis (RA) is a chronic autoimmune condition that affects not only your joints but also your overall immune and hormonal health. While conventional treatments often focus on managing pain and inflammation, they may not address the underlying causes. This is where Functional Medicine for Rheumatoid Arthritis comes in, taking a personalized, holistic approach to restore balance in your body. By combining nutrition, lifestyle, and lab-driven insights, you can finally target root causes instead of only suppressing symptoms. Hormone Reset is a specialized approach designed to complement functional medicine strategies and help support your overall health.
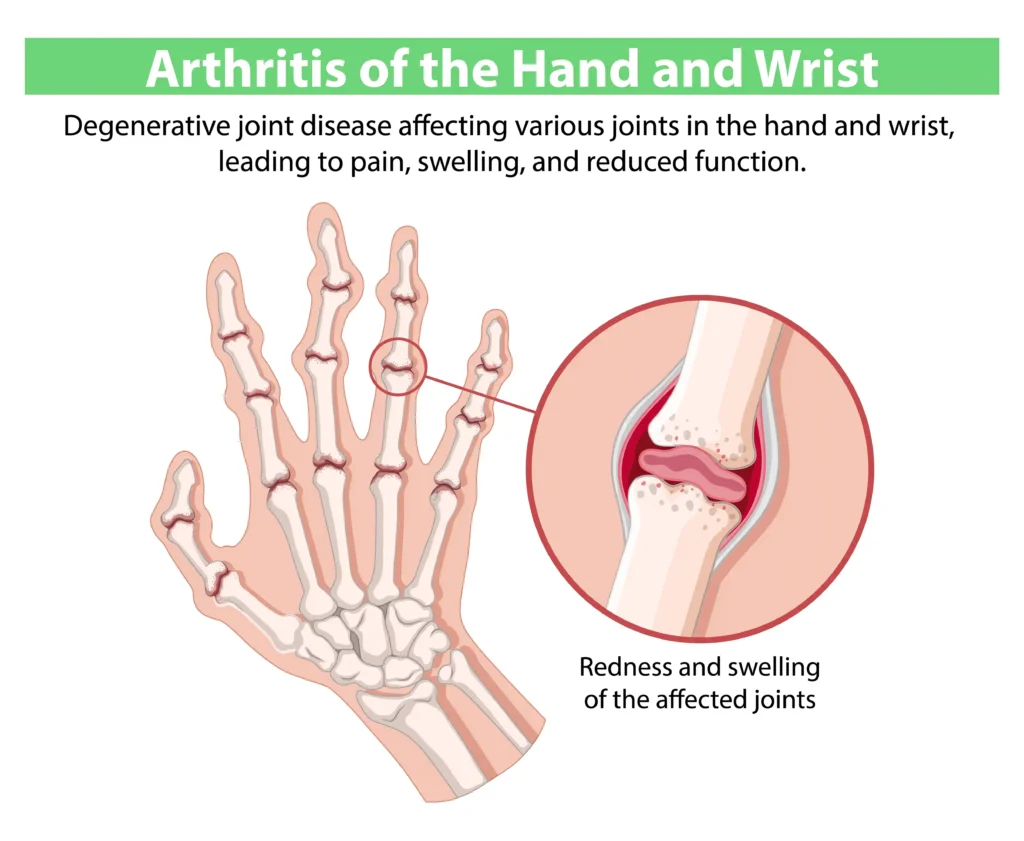
Understanding Rheumatoid Arthritis
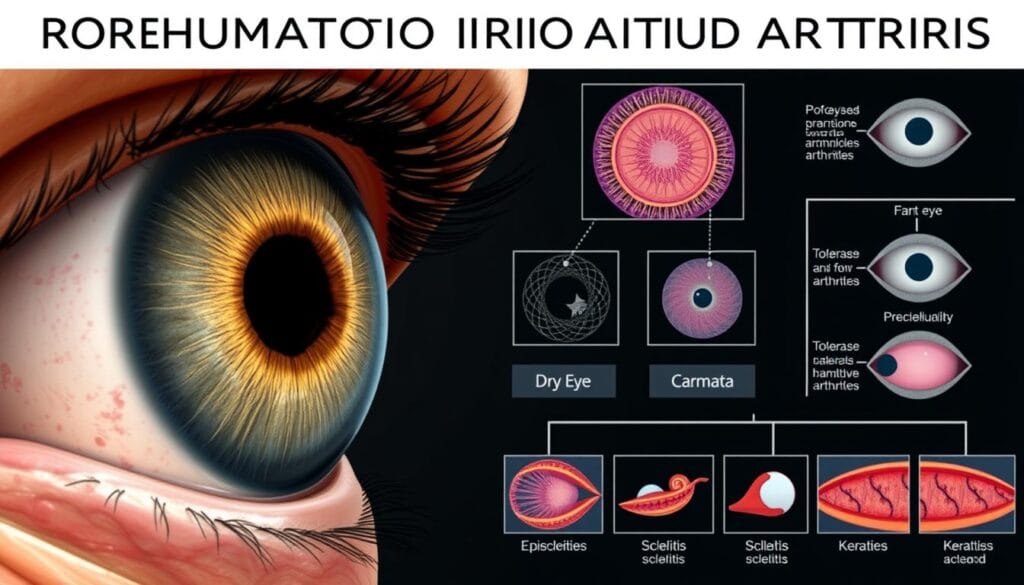
Rheumatoid Arthritis is an autoimmune condition where the immune system mistakenly attacks the lining of your joints, causing inflammation, pain, and stiffness. Symptoms can vary from mild discomfort to severe joint damage and fatigue. Chronic inflammation doesn’t only affect your joints — it can impact hormone regulation and overall energy levels.
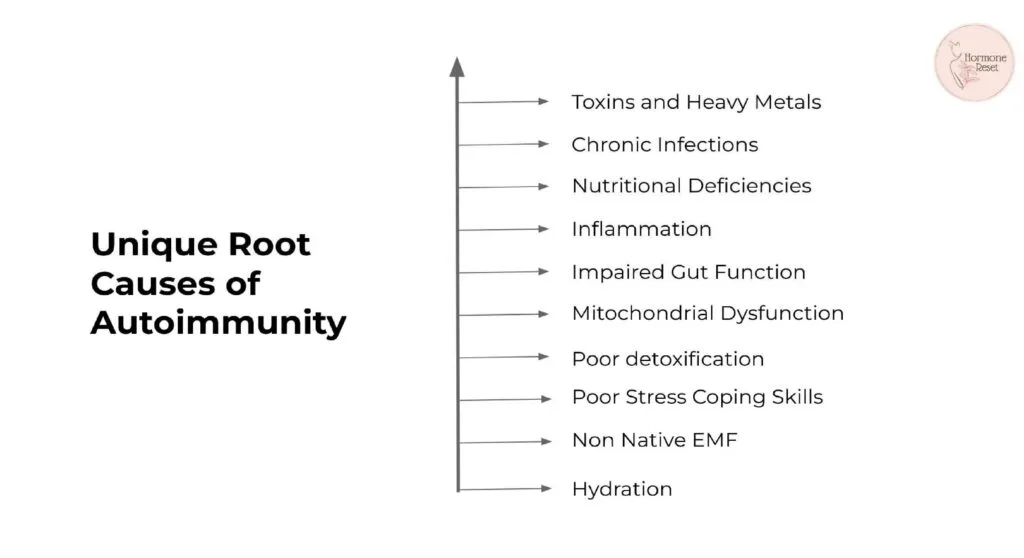
The connection between gut health, chronic inflammation, and autoimmune responses is critical. Research shows that intestinal permeability, gut microbiome imbalance, and certain food sensitivities can trigger immune dysregulation, making RA worse. Addressing these systemic factors is a cornerstone of Functional Medicine for Rheumatoid Arthritis.
Functional Medicine Approach to Rheumatoid Arthritis
Unlike conventional care that primarily focuses on symptom relief, Functional Medicine for Rheumatoid Arthritis emphasizes identifying and addressing root causes. This approach includes:
- Root-Cause Analysis: Understanding your unique triggers, such as dietary sensitivities, stress, environmental exposures, and genetic predisposition.
- Functional Lab Testing: Blood tests like CRP and ESR, autoantibodies like RF and anti-CCP, and advanced gut health assessments can provide a personalized picture of inflammation and immune activity.
- Personalized Treatment Plans: Based on lab results, lifestyle factors, and symptoms, plans can include nutrition, supplements, stress management, and targeted therapies.
This method allows practitioners to tailor interventions that support the immune system, reduce inflammation, and enhance hormonal balance — all part of a comprehensive functional medicine strategy.
Nutrition & Gut Health
Gut health plays a central role in autoimmune and inflammatory conditions. Dysbiosis, or an imbalance in gut microbiome, can exacerbate Arthritis by triggering systemic inflammation. Nutrition strategies focus on anti-inflammatory foods and avoiding common triggers:
Include:
- Omega-3 rich foods: salmon, chia seeds, flaxseeds
- Antioxidant-packed fruits and vegetables
- Turmeric, ginger, and other anti-inflammatory spices
Avoid:
- Refined sugars and processed foods
- Gluten and dairy if sensitive
- Trans fats and highly processed oils
A functional medicine diet plan can improve gut integrity, reduce inflammation, and support immune and hormonal balance by aligning perfectly with a Hormone Reset strategy.
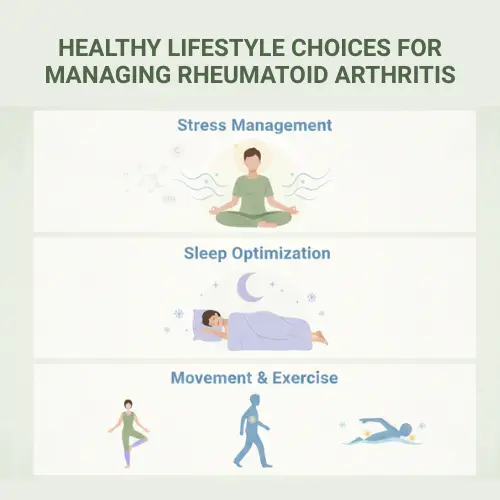
Healthy Lifestyle Choices for Managing Rheumatoid Arthritis
Lifestyle choices are powerful tools for managing Rheumatoid Arthritis and supporting functional medicine outcomes:
- Stress Management: Chronic stress elevates cortisol and can worsen autoimmune activity. Meditation, deep breathing, and mindfulness techniques are highly effective.
- Sleep Optimization: Quality sleep reduces inflammation and supports joint repair and hormonal health.
- Movement & Exercise: Low-impact activities such as yoga, walking, or swimming maintain joint mobility and reduce stiffness without aggravating inflammation.
Integrating these lifestyle practices enhances the effectiveness of Functional Medicine for Rheumatoid Arthritis while complementing the goals of Hormone Reset.
Hormone Reset: Supporting Functional Medicine for RA
While Functional Medicine for Rheumatoid Arthritis addresses root causes and immune modulation, Hormone Reset supports hormonal balance, energy levels, and metabolic health. Hormonal regulation plays a crucial role in inflammation control and immune resilience, making it a valuable adjunct for those managing RA.
- Personalized Hormone Support: Optimizes endocrine function to complement immune and joint health.
- Integrative Approach: Combines nutrition, lifestyle, and lab insights for comprehensive care.
- Enhanced Wellbeing: Supports energy, mood, and overall vitality while reducing inflammation.
By combining Hormone Reset with functional medicine, patients can experience a more holistic improvement in their RA symptoms and overall health.
Getting Started with Functional Medicine Rheumatoid Arthritis Care
- Consult a Functional Medicine Practitioner: They will assess your medical history, perform functional lab tests, and identify triggers.
- Develop a Personalized Plan: Integrating nutrition, lifestyle changes, and supportive therapies.
- Monitor Progress: Regular follow-ups and lab assessments ensure interventions are effective and adapted as needed.
- Support Hormonal Balance: Incorporate Hormone Reset principles to complement immune and joint health.
Taking a structured, evidence-based approach ensures that every aspect of RA management is addressed — from reducing inflammation to optimizing hormones.
Frequently Asked Questions (FAQs)
1. How does Functional Medicine treat Rheumatoid Arthritis?
Functional Medicine treats Rheumatoid Arthritis by addressing the root causes of inflammation and immune system imbalance rather than only managing symptoms. It uses personalized lab testing, nutrition strategies, lifestyle interventions, and hormone support to reduce joint pain, improve mobility, and restore overall health naturally.
2. How can Hormone Reset support Functional Medicine for Rheumatoid Arthritis?
Hormone Reset complements Functional Medicine for Rheumatoid Arthritis by optimizing endocrine function, which helps regulate inflammation, improve immune responses, and enhance energy levels. Combined with dietary changes, gut health strategies, and lifestyle interventions, Hormone Reset supports better joint function and overall well-being
3. What dietary changes help reduce Rheumatoid Arthritis symptoms naturally?
A diet that supports Functional Medicine care focuses on anti-inflammatory foods, including omega-3-rich fish, leafy greens, berries, turmeric, and ginger. Avoiding processed foods, refined sugars, gluten, and dairy (if sensitive) can help reduce systemic inflammation and improve both joint and hormonal health.
4. What lifestyle interventions are recommended for Functional Medicine Rheumatoid Arthritis care?
Lifestyle practices play a crucial role in managing Rheumatoid Arthritis through Functional Medicine. Stress reduction, quality sleep, low-impact exercises like yoga, swimming, or walking, and mindfulness techniques all help control inflammation, support hormone balance, and maintain joint mobility naturally.
5. How do I get started with Functional Medicine for Rheumatoid Arthritis?
Consult a qualified practitioner who can perform functional lab testing, identify root causes, and create a personalized treatment plan. Incorporating Hormone Reset strategies further supports immune and hormonal health, helping you achieve long-term symptom relief and improved quality of life.
Conclusion
Functional Medicine for Rheumatoid Arthritis provides a holistic, personalized approach that goes beyond symptom management. By addressing root causes such as gut dysbiosis, dietary triggers, stress, and hormonal imbalances, patients can experience lasting relief, improved mobility, and better overall health. Integrating Hormone Reset strategies enhances functional medicine outcomes, supporting both immune and endocrine function.
Take control of your health today with a comprehensive, functional medicine approach that truly targets the underlying causes of Rheumatoid Arthritis.
👉 Address the root causes of Rheumatoid Arthritis. Start your functional medicine journey today.

References
- Integrative Approaches to the Testing and Treatment of Rheumatoid Arthritis– Rupa Health
- Rheumatoid Arthritis: How a Functional Medicine Approach Can Ease Your Sore, Achy Joints– Max Well Clinic
- Rheumatoid arthritis: reducing inflammation and addressing underlying triggers– Melbourne Functional Medicine
- What is Rheumatoid Arthritis, and how can Functional Medicine help?- Surrey Centre for Nutrition
- A Functional Medicine Guide To Rheumatoid Arthritis– Dr. Will Cole
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset