A Functional Medicine Guide to Hormonal Healing Through Tiny Foods
Table of Contents
PCOS: Not a Hormone Problem — A Body in Survival Mode
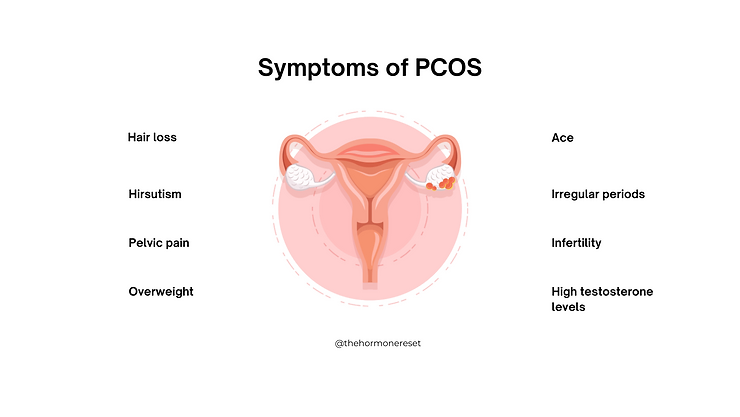
Polycystic Ovary Syndrome (PCOS) is often misunderstood as a female hormone disorder — but in reality, PCOS is the body’s intelligent survival response to long‑standing internal stress.
Your ovaries are not faulty.
Your hormones are not confused.
Your body is adapting.
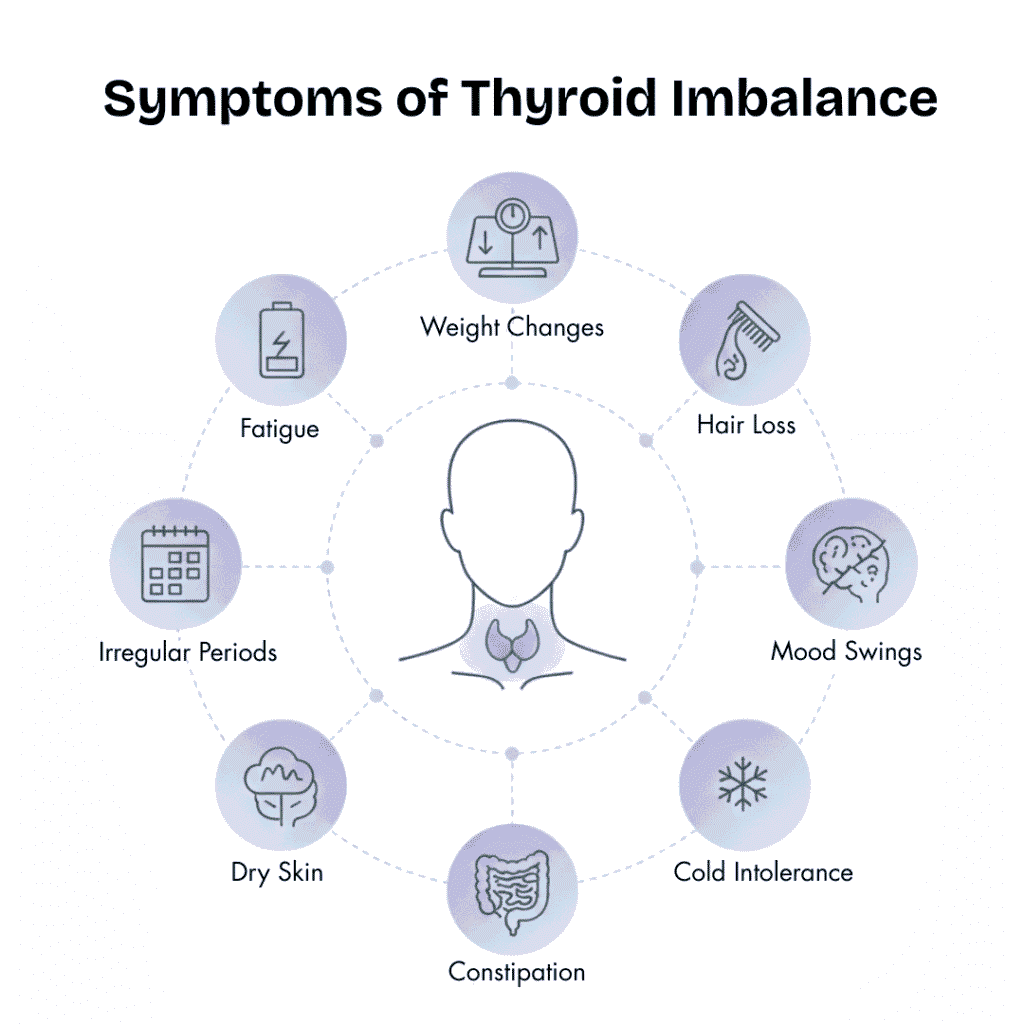
PCOS develops when the body feels unsafe at a metabolic level — from blood sugar swings, chronic inflammation, gut imbalance, nutrient depletion, emotional stress, and poor detoxification. Ovulation becomes irregular, progesterone drops, and androgens rise — not as a mistake, but as an adaptive strategy.
That is why symptoms such as irregular periods, acne, weight gain, hair fall, infertility, anxiety, fatigue, or PMS are not isolated problems. They are messages.
Treating PCOS by only inducing periods or suppressing hormones may silence the symptoms temporarily, but it never answers the most important question:
Why did the body choose this pattern in the first place?
This is exactly where Functional Medicine begins.
The Functional Medicine Approach to PCOS
Functional Medicine asks a different question: “Why did the body shift into this hormonal pattern?”
From this perspective, PCOS is a systems imbalance, involving:
- Gut–liver–hormone axis
- Insulin–ovary–androgen loop
- Stress–adrenal–progesterone pathway
- Inflammatory and immune signals
Healing PCOS means restoring:
- Insulin sensitivity
- Estrogen clearance
- Ovulation rhythm
- Nutrient sufficiency
- Nervous system safety
Here, food is not just nutrition — it is biological information.
And among the most powerful yet underrated foods for PCOS are seeds.
Why Seeds Are Powerful in PCOS
Seeds are tiny, but they are hormonally intelligent. They contain:
- Soluble & insoluble fiber
- Essential fatty acids
- Minerals like zinc, magnesium, and iron
- Phyto‑compounds that influence estrogen metabolism
From a functional medicine lens, seeds:
- Improve gut health
- Support liver detox pathways
- Reduce inflammation
- Stabilize blood sugar
- Nourish ovulation and progesterone
They don’t force the body — they guide it gently back into rhythm.
Seed‑by‑Seed Guide for PCOS Healing

Flax Seeds (Alsi) — The Estrogen Detoxifier
Functional role:
- Rich in lignans → bind excess estrogen
- Reduce beta‑glucuronidase activity
- Improve estrogen clearance via stool
Benefits in PCOS:
- Regulates cycles
- Reduces estrogen dominance
- Improves acne & hair fall
- Relieves constipation
How to use:
- Freshly ground only
- 1–2 tbsp daily, preferably morning

Chia Seeds — The Insulin Stabilizer
Functional role:
- Forms gel → slows glucose absorption
- Improves insulin sensitivity
- Feeds beneficial gut bacteria
Benefits in PCOS:
- Controls cravings
- Supports weight balance
- Improves energy & bowel movements
How to use:
- Always soaked (20–30 min)
- 1 tbsp daily

Hemp Seeds — The Hormone Nourisher
Functional role:
- Complete plant protein
- Ideal omega‑6 : omega‑3 ratio
- Rich in magnesium & zinc
Benefits in PCOS:
- Improves ovulation quality
- Supports progesterone
- Reduces fatigue & hair thinning
How to use:
- Raw, no soaking
- 1 tbsp daily

Pumpkin Seeds — The Androgen Modulator
Functional role:
- High in zinc
- Supports insulin signaling
- Anti‑inflammatory
Benefits in PCOS:
- Reduces acne & hirsutism
- Improves follicle development
How to use:
- 1 tbsp soaked or lightly roasted

Sunflower Seeds — The Progesterone Supporter
Functional role:
- Rich in vitamin E
- Supports corpus luteum
- Antioxidant for ovaries
Benefits in PCOS:
- Improves luteal phase
- Reduces PMS & breast tenderness
How to use:
- 1 tbsp raw or lightly roasted

Sesame Seeds (Til) — The Uterine Warmer
Functional role:
- Rich in calcium, iron & lignans
- Improves uterine blood flow
Benefits in PCOS:
- Helpful in delayed periods
- Supports implantation
Note: Avoid during heavy bleeding or severe estrogen dominance.
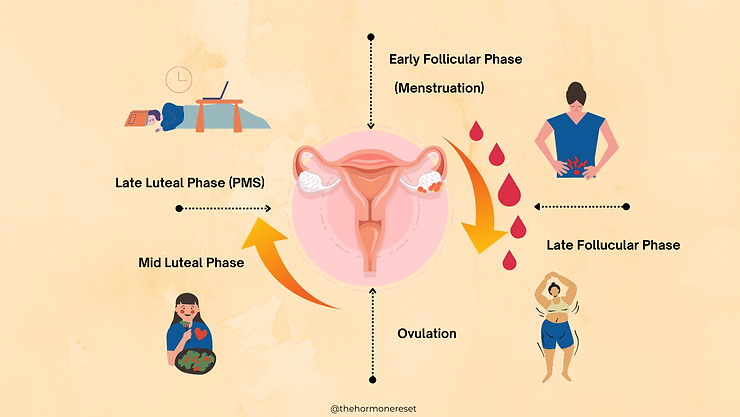
Seed Cycling & Rotation in PCOS
Seed cycling aligns nutrition with hormonal rhythm.
Follicular Phase (Day 1–14)
- Flax seeds
- Pumpkin seeds
Purpose: Estrogen balance & follicle growth
Luteal Phase (Day 15–28)
- Sunflower seeds
- Sesame seeds
Purpose: Progesterone support & PMS reduction
For irregular cycles: Follow moon cycle (new moon to full moon = follicular seeds).
Practical Ways to Add Seeds Daily
- Hormone detox water (chia + flax)
- Smoothies with hemp & pumpkin seeds
- Seed chutney or podi with meals
- Seed ladoos with dates & nuts
- Coconut yogurt with soaked chia
- Roasted seed trail mix
Consistency matters more than quantity.
Important Clinical Points
- Start slow if bloating, IBS or SIBO present
- Prefer soaked or ground forms
- Use fresh & organic seeds
- Avoid excess during acute gut inflammation
Seeds support healing — but PCOS still needs stress regulation, sleep, protein adequacy, and gut repair.
Frequently Asked Questions
1. Can seeds really help manage PCOS symptoms naturally?
Yes, when used consistently and correctly, seeds can support PCOS management. From a functional medicine perspective, seeds provide fiber, healthy fats, minerals, and phyto-compounds that help regulate blood sugar, improve estrogen clearance, reduce inflammation, and support ovulation. They do not “cure” PCOS overnight, but they create the internal conditions needed for hormonal balance.
2. How long does it take to see results from seed cycling in PCOS?
Most women begin to notice subtle improvements such as better digestion, reduced cravings, improved energy, or less PMS within 4 to 6 weeks. Menstrual regularity, acne reduction, or ovulation support may take 2 to 3 cycles. Consistency matters more than quantity, and results depend on overall lifestyle, stress levels, and metabolic health.
3. Is seed cycling safe for women with irregular or missing periods?
Yes. For women with irregular cycles or absent periods, seed cycling can be followed according to the moon cycle or simply rotated every 14 days. Seeds are food, not hormones, and they gently support the body’s rhythm rather than forcing ovulation. However, women with severe gut issues or active inflammation should start slowly and seek guidance.
4. Can seeds replace medication or hormonal treatment for PCOS?
Seeds are a supportive therapy, not a replacement for medical care when it is needed. Functional nutrition works best alongside proper diagnosis, stress management, sleep, adequate protein intake, and, when required, medical treatment. Seeds help address root causes like insulin resistance and estrogen imbalance, but should be part of a comprehensive approach.
5. Are there any situations where seed intake should be limited in PCOS?
Yes. Women with active IBS, SIBO, severe bloating, or acute gut inflammation should introduce seeds gradually and prefer soaked or ground forms. Excessive intake without adequate hydration may worsen digestion. Also, sesame seeds should be limited during heavy menstrual bleeding or severe estrogen dominance.
Final Conclusion
PCOS is not a failure of the body. It is a request for safety, nourishment, and rhythm.
Seeds may be small, but when used daily and intentionally, they deliver powerful messages:
You are nourished.
You are safe.
You can ovulate.
You can heal.
Sometimes, hormonal healing doesn’t begin with strong medicine — It begins with tiny seeds and daily rituals
If you are a woman with PCOS, remember: your body is not broken. It is listening. And what you feed it matters.

References
- Polycystic ovary syndrome– PubMed
- Polycystic ovary syndrome: definition, aetiology, diagnosis and treatment– National Library of Medicine
- Erythema nodosum-like panniculitis mimicking disease recurrence– National Library of Medicine
- Mesenchymal stem cells in the osteosarcoma microenvironment– National Library of Medicine
- Antidepressant use before and after the diagnosis of type 2 diabetes- National Library of Medicine
- A subclavian artery injury, secondary to internal jugular vein cannulation, is a predictable right-sided phenomenon– National Library of Medicine
- Reading and listening in people with aphasia: effects of syntactic complexity– National Library of Medicine
- Mycotoxins, Phytoestrogens and Other Secondary Metabolites in Austrian Pastures: Occurrences, Contamination Levels and Implications of Geo-Climatic Factors– National Library of Medicine
- A Taste-intensity Visual Analog Scale: An Improved Zinc Taste-test Protocol– National Library of Medicine
- Facile production of chitin from crab shells using ionic liquid and citric acid– National Library of Medicine
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset