The Growing Burden of Autoimmune Conditions
Autoimmune diseases affect millions worldwide, where the immune system mistakenly attacks healthy tissues. Conditions like Hashimoto’s thyroiditis, lupus, and psoriasis are particularly concerning due to their chronic nature and complex symptoms.
While genetics may play a role in some, environmental triggers often serve as the catalysts that initiate or exacerbate them. In this blog, we explore how environmental factors influence autoimmune conditions such as Hashimoto’s thyroiditis, lupus, and psoriasis and how understanding these triggers can help not only in managing these diseases but in reversing them.
Why This Matters?
Imagine living with unrelenting fatigue, joint pain, or skin lesions that affect your physical and emotional well-being. Now, consider the confusion of managing these symptoms when no clear cause is evident. That’s the reality for many with autoimmune conditions.
Environmental triggers often go unnoticed, yet they can significantly influence disease progression. Various factors like the foods we eat, the stress we endure, and the harmful chemicals we encounter daily can tip the immune system into overdrive, exacerbating these conditions. Understanding these connections is vital to addressing autoimmune diseases effectively.
What are some Environmental Triggers in Autoimmune Conditions?
1. Diet and Digestive System Health and Autoimmune Diseases
Diet can profoundly impact autoimmune conditions by influencing inflammation, gut health, and immune regulation.
- Leaky Gut Syndrome:
Many autoimmune diseases are linked to increased intestinal permeability, or “leaky gut,” where toxins and undigested food particles enter the bloodstream. This triggers an immune response, worsening conditions like Hashimoto’s and lupus. - Case Study: Hashimoto’s Thyroiditis
A 2017 study in Thyroid Research highlighted the benefits of eliminating gluten for patients with Hashimoto’s. Gluten shares molecular similarities with thyroid tissue, leading to cross-reactivity and immune attacks on the thyroid.- Result: Patients who adopted a gluten-free diet reported reduced thyroid antibody levels and improved symptoms.
- Pro-inflammatory Foods:
Diets high in processed foods, sugar, and trans fats promote inflammation, aggravating psoriasis and lupus symptoms. Conversely, anti-inflammatory diets rich in omega-3 fatty acids, antioxidants, and fiber help manage these diseases.
2. Stress and Autoimmune Diseases
Chronic stress is a known disruptor of immune function. Stress increases cortisol levels, which can impair immune regulation and exacerbate autoimmune flares.
- Case Study: Lupus (Systemic Lupus Erythematosus)
In a 2019 study published in Arthritis Care & Research, patients with lupus who reported high-stress levels experienced more frequent disease flares and greater organ involvement.- Result: Implementing stress management techniques, such as mindfulness and yoga, helped stabilise her condition over time.
3. Toxins and Autoimmune Diseases
Environmental toxins, including heavy metals, pesticides, and household chemicals, can act as triggers by disrupting the immune system.
- Toxic load and immune dysregulation:
Persistent exposure to toxins increases oxidative stress and inflammation, which may lead to autoimmunity. For instance, mercury exposure from contaminated fish has been linked to autoimmune diseases like lupus. - Case Study: Psoriasis
Research in Clinical and Experimental Dermatology found that patients with psoriasis often had higher levels of environmental toxins, such as dioxins and phthalates, in their bodies.- Result: Reducing exposure to such toxins, alongside phototherapy and anti-inflammatory diets, improved skin lesions in many cases.
4. Infections and Autoimmune Diseases
Infections play a significant role in the development and exacerbation of autoimmune diseases. Through mechanisms like molecular mimicry, bystander activation, and chronic immune stimulation, infections can lead the immune system to mistakenly attack the body’s tissues.
- Epstein-Barr virus (EBV) is closely linked to conditions such as systemic lupus erythematosus (SLE) and multiple sclerosis (MS). At the same time, streptococcal infections are known to trigger guttate psoriasis and rheumatic fever. Chronic infections, such as those caused by Helicobacter pylori or Mycoplasma, can create persistent inflammation that heightens the risk of autoimmune responses. Understanding and managing these infection-autoimmune links is critical for reducing flare-ups and improving long-term outcomes in affected individuals.
Also Read: Impact of Autoimmune Disorders on Skin Health
Bridging the Gaps: What Science and Case Studies Tell Us
While autoimmune diseases like Hashimoto’s, lupus, and psoriasis differ in their manifestations, they share common pathways influenced by environmental triggers. The interplay between diet, stress, and toxins is critical to both the onset and progression of these diseases.
Key Insights from Research:
- Personalised Nutrition:
Adopting diets tailored to individual sensibilities, such as gluten-free for Hashimoto’s or anti-inflammatory for lupus and psoriasis, can alleviate symptoms. - Stress Management:
Practices like meditation, cognitive behavioural therapy, and regular physical activity help mitigate the effects of chronic stress on autoimmune flares. - Reducing Toxic Exposure:
Switching to organic produce, avoiding processed foods, and using non-toxic household products can reduce the toxic burden on the body, potentially improving disease outcomes.
Functional Medicine Approach to Reversing Autoimmune Conditions
The functional medicine approach focuses on identifying and addressing the root causes of autoimmune diseases rather than merely managing symptoms. Here’s a breakdown of how functional medicine reverses autoimmune conditions:
1. Comprehensive Evaluation
- Medical History and Genetics: Reviewing family history and personal health milestones to uncover predispositions and triggers.
- Environmental Factors: Evaluating exposure to toxins, infections, and stress.
- Lifestyle Assessment: Analyzing diet, sleep, exercise, and mental health habits.
2. Root Cause Identification
- Gut Health: A significant focus is placed on intestinal permeability, or “leaky gut,” which allows antigens to trigger an immune response.
- Food Sensitivities: identifying and eliminating common triggers like gluten, dairy, and processed foods.
- Toxins: Assessing for heavy metals, mould, or chemical exposures.
- Infections: Testing for underlying viral, bacterial, or parasitic infections that may contribute to immune dysfunction.
3. Personalized Dietary Interventions
- Elimination Diets: Remove potential inflammatory foods and gradually reintroduce them to identify sensitivities.
- Nutrient-dense diet: A nutrient-dense diet focusing on anti-inflammatory foods such as vegetables, healthy fats, and quality proteins
- Gut-Healing Foods: Incorporating hydrolysed protein, bone broth, and prebiotic-rich vegetables to support microbiome health.
4. Stress Management and Emotional Health
- Chronic stress can exacerbate inflammation and immune dysregulation. Stress-reduction strategies include:
- Mindfulness and meditation.
- Cognitive Behavioral Therapy (CBT).
- Breathing exercises and yoga.
- Addressing past trauma through therapeutic interventions.
5. Targeted Nutritional Support
Functional medicine practitioners often recommend supplements based on individual needs:
- Omega-3 Fatty Acids: To reduce inflammation.
- Vitamin D: For immune modulation.
- Probiotics: To support gut microbiota balance.
- Zinc, Selenium, and Magnesium: Essential for proper immune function.
- Curcumin and Resveratrol: Natural anti-inflammatory agents.
6. Detoxification and Environmental Changes
- Supporting liver detox pathways through a clean diet and supplements like milk thistle.
- Reducing environmental toxin exposure by:
- Using clean, natural products for personal care and home.
- Avoiding plastic and BPA exposure.
- Filtering water and air.
7. Movement and Physical Activity
- Regular exercise improves hormonal health by reducing stress, improving circulation, and enhancing lymphatic drainage without overburdening the body.
- Gentle activities like walking, yoga, or tai chi are often recommended for those with active inflammation.
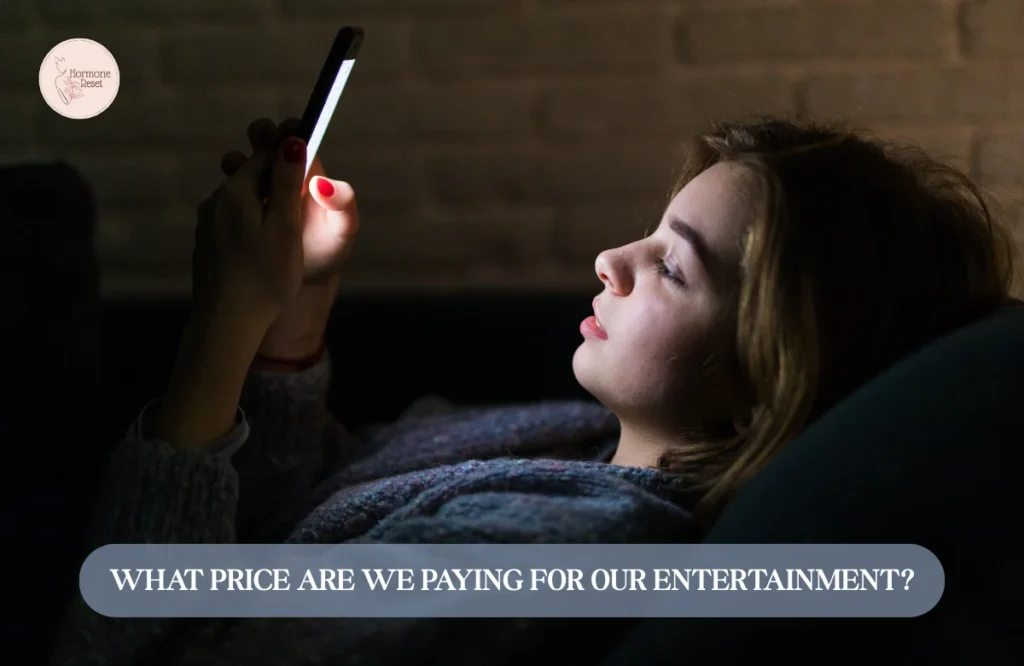
8. Restoring Circadian Rhythm
- Prioritising sleep hygiene to ensure restorative rest, which is critical for healing and immune regulation.
- Strategies include:
- Consistent sleep schedules.
- Limiting screen time before bed.
- Creating a dark, cool, and quiet sleep environment.
9. Monitoring and Adjustment
Functional medicine emphasises regular follow-ups to monitor progress and adjust treatment plans as needed. Testing is often repeated to evaluate changes in inflammatory markers, gut health, and immune system activity.
The Goal: Balance and Restoration
The functional medicine approach seeks to restore balance to the immune system by addressing the underlying triggers of autoimmunity. By tailoring interventions to the individual’s needs, this approach offers the potential not just to manage but to reverse autoimmune conditions and promote long-term health.
Would you like guidance on implementing these principles or resources for specific autoimmune conditions?
Taking Control of Your Health
Environmental triggers, such as diet, stress, and toxins, play a significant role in autoimmune diseases like Hashimoto’s, lupus, and psoriasis. While genetics set the stage, lifestyle factors often determine the severity of the condition.
By adopting an anti-inflammatory diet, managing stress, and reducing exposure to toxins, patients can take proactive steps toward managing their symptoms and improving their quality of life.
References:
- Fasano, A. (2012). “Leaky gut and autoimmune diseases.” Clinical Reviews in Allergy & Immunology. https://link.springer.com/article/10.1007/s12016-012-8290-4
- Li, Y., et al. (2017). “Gluten-free diet and its impact on Hashimoto’s thyroiditis.” Thyroid Research. https://thyroidresearch.biomedcentral.com/articles/10.1186/s13044-017-0147-5/
- Sterling, K. A., et al. (2019). “Stress and disease activity in lupus.” Arthritis Care & Research. https://onlinelibrary.wiley.com/doi/abs/10.1002/acr.23960
- Kimball, A. B., et al. (2018). “Environmental triggers in psoriasis.” Clinical and Experimental Dermatology. https://onlinelibrary.wiley.com/doi/full/10.1111/ced.13683
- Ricker MA, Haas WC. Anti-inflammatory diet in clinical practice: a review. Nutr Clin Pract. 2017;32(3):318-325. doi:10.1177/0884533617700353
- How to use food to help your body fight inflammation. Mayo Clinic. Published August 13, 2019. Accessed February 26, 2021. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/how-to-use-food-to-help-your-body-fight-inflammation/art-20457586
- Fasano, A. (2020). Leaky gut and autoimmune diseases. Clinical Reviews in Allergy & Immunology, 58(3), 384-396.
- Leung, A. M., Braverman, L. E., & Pearce, E. N. (2012). History of U.S. iodine fortification and supplementation. Nutrients, 4(11), 1740-1746.
- Proal, A. D. (2017). Infection and autoimmunity. Nature Reviews Rheumatology, 13(4), 196-198.
- Rose, N. R., & McGuire, K. L. (2018). Environmental triggers of autoimmunity. Annual Review of Medicine, 69, 287-299.
- Schug, T. T., Janesick, A., et al. (2011). Endocrine-disrupting chemicals and disease susceptibility. Journal of Steroid Biochemistry and Molecular Biology, 127(1-2), 204-215.
- Tsokos, G. C. (2011). Systemic lupus erythematosus. New England Journal of Medicine, 365(22), 2110-2121.
Share


Leave a Reply