Rheumatoid arthritis (RA) is a chronic autoimmune disease where the immune system attacks the synovial membranes of joints, causing pain, inflammation, and deformity. It most commonly affects individuals aged 30-50 and is three times more prevalent in women than men. It is a long-term condition that causes pain, swelling, and stiffness in the joints.
If you’ve been diagnosed, chances are, you’ve been prescribed medications to manage it. But is that really the best solution? While medications can help manage symptoms, they dont offer a lasting solution. Let’s explore why medications may not be the ultimate answer for RA.
The Problem: Medications Can’t Reverse Rheumatoid Arthritis
When you’re diagnosed with rheumatoid arthritis, the first line of defense often involves medications like nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), and biologics. These medications aim to slow down the progression of the disease, reduce inflammation, and relieve pain. But here’s the problem: they don’t cure RA. In fact, they’re only designed to manage or suppress the symptoms.
A 2017 study published in the Journal of Rheumatology showed that while DMARDs can reduce joint inflammation and slow disease progression, only 30-40% of patients achieved remission after using these medications for a year. This means the majority of people are still living with significant symptoms even while on medication.
Additionally, medications often come with a slew of side effects. Long-term use of NSAIDs, for example, has been linked to stomach ulcers, liver damage, and increased risk of heart attacks. Biologics can suppress the immune system, making patients more vulnerable to infections.
Agitation: The Limits and Risks of Medication Dependence
It’s easy to feel like medications are the only way to keep rheumatoid arthritis in check. But relying solely on pharmaceuticals comes with risks and limitations. For starters, medications don’t address the underlying cause of RA, which is the reason why the immune system is attacking the joints.
A long-term reliance on drugs may mask the symptoms while the disease continues to progress. According to a case study published in Rheumatology International, one patient who had been on DMARDs for five years experienced decreased effectiveness of the drugs over time. By the end of the case study, they still had joint deterioration and required joint replacement surgery despite ongoing medication.
The risks don’t stop there. Many RA drugs also carry potential long-term health risks. A 2020 study in The Lancet found that patients on biologics were 60% more likely to develop serious infections due to immune suppression. Medications may temporarily control RA symptoms, but at what cost to your overall health?
Solution: What You Can Do Instead of Relying Solely on Medication
Today, science has a pretty good understanding of the reasons that lead the immune system to attack the joints. RA is driven by an imbalance in immune cells, with an excess of Th1 lymphocytes producing inflammatory mediators and a deficiency of Th2 lymphocytes. The question we have to ask is – why is this imbalance happening?
Environmental factors, such as viral and bacterial infections, play a key role by triggering chronic inflammation and oxidative tissue damage. These infections can also compromise gut health, leading to intestinal permeability, low Secretory IgA, elevated zonulin, and other inflammatory bowel markers, which may further exacerbate the autoimmune response.
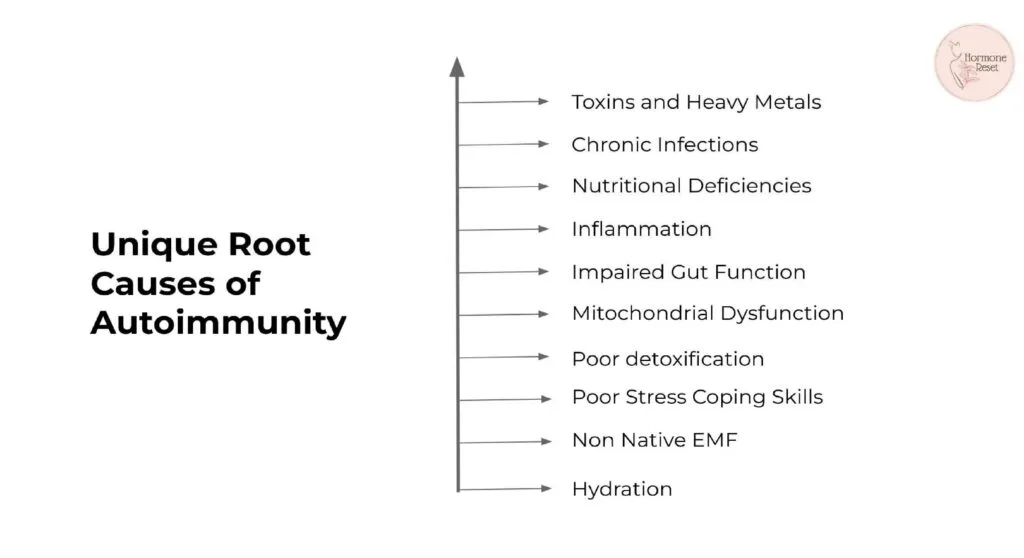
Key contributors include:
- Nutritional deficiencies: Low levels of essential nutrients like vitamin D, vitamin A, omega-3 fatty acids, and antioxidants, amongst many others, can weaken immune regulation and joint health.
- Chronic infections: Overgrowth of bacteria, fungi, parasites, viruses, etc in the body can trigger immune dysfunction leading to autoimmunity.
- Gut health imbalance: Increased intestinal permeability (“leaky gut”) allows toxins and undigested food particles to enter the bloodstream, triggering autoimmune responses.
- Reactivity to triggers: Chemicals, pathogens, or certain foods can provoke immune responses and cross-reactivity, leading to inflammation and worsening symptoms.
- Toxins: A variety of toxins, including heavy metals, bacterial and fungal toxins, and agricultural and other environmental toxins, are known to trigger the immune system into hypervigilance and then autoimmunity.
- Stress or trauma: Chronic or acute stress can disrupt the body’s stress response, promote inflammation, and act as a trigger for RA onset or exacerbation.
The rising prevalence of autoimmune diseases is linked to gut health. A compromised intestinal barrier and immune system reactivity to food are major contributors to immune system overstimulation and disease progression. Addressing gut health through personalised dietary strategies that reduce food triggers, alongside targeted care, is essential for recovery.
A Functional Medicine approach emphasizes addressing these factors through personalized nutrition, gut healing, stress management, detoxification, addressing chronic infections, and identifying specific triggers to manage RA effectively. These alternative strategies can help you manage symptoms and potentially reverse the disease’s progression without relying entirely on pharmaceuticals. Some of these are discussed below.
- Anti-Inflammatory Diet: Numerous studies have shown that diet plays a critical role in reducing inflammation. One study in Arthritis Care & Research found that RA patients who followed an anti-inflammatory diet rich in omega-3 fatty acids, fresh fruits, and vegetables experienced reduction in flare-ups and improved overall joint health.
Eliminate all processed foods, gluten, dairy and sugars, as they can trigger inflammation. Work with an experienced Functional nutritionist to personalise your diet based on your symptoms and test results. - Physical Therapy and Exercise: Regular, low-impact exercise can improve joint flexibility and reduce pain. According to the American College of Rheumatology, exercises such as swimming, yoga, and walking can strengthen the muscles surrounding the joints, alleviating pressure and improving mobility.
Physical therapy has also been shown to reduce reliance on pain medications. A case study published in Physical Therapy & Rehabilitation Journal highlighted a patient who significantly reduced NSAID usage after participating in a targeted physical therapy program for six months. - Stress Management: RA symptoms often worsen during periods of high stress. Mind-body practices like meditation, deep breathing exercises, and progressive muscle relaxation have been proven to reduce stress and, in turn, lessen inflammation.
A 2018 study in Psychosomatic Medicine found that RA patients who practiced mindfulness meditation for eight weeks saw measurable reductions in inflammatory markers, compared to those who relied on medications alone. - Supplements and Natural Remedies: Supplements form an integral part of the Functional Medicine approach to treating RA. Various supplements and nutraceuticals like Evening Primrose Oil (GLA), Boswellia, Collagen, Turmeric, etc. have been shown to offer significant benefits in RA.
Be sure to consult with your healthcare provider before adding any supplements to your routine.
The Power of Holistic Treatment
While we have helped many patients with RA, one case of an athlete who used to run marathons stands out. This patient was told that her running days were over as she could not even walk properly due to the pain caused by her inflamed knees. After working with us for six months, not only could she get back to running, but she broke her personal records! In other words, not only did her RA reverse, but her health, stamina and fitness improved so much that she could break her personal records.
Take Action Today
Medications can help control rheumatoid arthritis symptoms, but they aren’t a cure, and long-term dependence on them can carry risks. The good news is functional medicine can help by making lifestyle changes, including dietary modifications, stress management, and supplementation so that you can take control of your RA and reduce your reliance on medications. Empower yourself by taking small steps toward a healthier, more balanced approach to RA care.

References:
- Jasvinder A Singh, Treatment Guidelines in Rheumatoid Arthritis, Published by Elsevier Inc., 2022 Jul 5, https://pubmed.ncbi.nlm.nih.gov/35953230/
- Bicer, A., Tursen, U., Cimen, O. et al. Prevalence of dermatophytosis in patients with rheumatoid arthritis. Rheumatol Int 23, 37–40 (2003). https://doi.org/10.1007/s00296-002-0238-3
- Tedeschi SK, Frits M, Cui J, Zhang ZZ, Mahmoud T, Iannaccone C, Lin TC, Yoshida K, Weinblatt ME, Shadick NA et al.. Diet and rheumatoid arthritis symptoms: survey results from a rheumatoid arthritis registry. Arthritis Care Res (Hoboken)
- Gioxari A, Kaliora AC, Marantidou F, Panagiotakos DP. Intake of omega-3 polyunsaturated fatty acids in patients with rheumatoid arthritis: a systematic review and meta-analysis.
- Exercise & Arthritis, American College of Rheumatology, April 2023 by Howard Yang, MD,
- 2022 American College of Rheumatology (ACR) Guideline for Exercise, Rehabilitation, Diet, and Additional Integrative Interventions for Rheumatoid Arthritis, 2023 Aug
- The Journal of Rheumatology in 2017, which evaluated the effectiveness of disease-modifying antirheumatic drugs (DMARDs)
- Psychosomatic Medicine, 2018: A study demonstrating RA patients practicing mindfulness meditation
- The Journal of Clinical Rheumatology, 2021: A review on turmeric supplementation
Share


