Table of Contents
We live in a world where entertainment never sleeps.
A screen lights up our mornings, keeps us company through the day, and often lulls us to sleep at night. We tell ourselves it’s harmless — a few episodes, a quick scroll, a game or two. But beneath this comfort lies a silent trade-off: our health, focus, and biological balance are paying the price.
Let’s uncover how our beloved devices are reshaping our health — system by system — and how a functional medicine approach can help us restore balance.
1. Eyes — When Screens Steal Our Vision
It starts with a familiar feeling: tired eyes, blurred vision, that dull ache behind the forehead after a long day online. This is what experts call Digital Eye Strain (DES) — a result of prolonged near-focus and reduced blinking.
Studies by the American Academy of Ophthalmology (AAO) show that people blink nearly 60% less when staring at screens, leading to dryness, irritation, and even redness.
Over time, continuous close-up focus can alter how the eye grows — especially in children — raising the risk of myopia (nearsightedness).
And while the idea that screens literally “burn” our retinas is exaggerated, research suggests that blue light—particularly from LED lighting and digital screens (phones, laptops, tablets, monitors)—can increase oxidative stress in retinal cells, making the eyes more vulnerable to inflammation and mitochondrial dysfunction.
Mechanisms & implications
1. Blue light & retinal mitochondrial stress
LEDs and screens emit a higher proportion of short-wavelength blue light (≈400–490 nm), also referred to as high-energy visible (HEV) light. This wavelength penetrates deep into the eye and is absorbed by retinal photoreceptors and retinal pigment epithelial (RPE) cells. Excessive exposure may increase reactive oxygen species (ROS), stressing retinal mitochondria and potentially leading to cumulative, sub-clinical retinal damage over time. While this does not equate to immediate injury, it may contribute to long-term vulnerability to age-related retinal disorders, especially in individuals with low antioxidant reserves or existing metabolic stress.
2. Prolonged near-focus & visual strain
Screens are typically viewed at 30–40 cm, requiring sustained accommodative and convergence effort. Prolonged near-work can fatigue the ciliary muscles and extraocular muscles, contributing to symptoms such as eye strain, headaches, and blurred vision.
3. Reduced blink rate & dry eye symptoms
During focused screen use, blink rate may drop by 40–60%, leading to tear film instability, increased tear evaporation, and dry eye symptoms (burning, grittiness, and redness). Air-conditioned environments and prolonged indoor screen use further worsen this effect.
4. Myopia risk: association, not simple causation
The link between screen use and myopia likely reflects multiple interacting factors, not screen time alone. These include:
- Increased near-work duration
- Reduced outdoor light exposure (which is protective for eye growth regulation)
- Limited distance viewing
- Genetic susceptibility
5. Circadian & repair implications (often overlooked)
Evening blue-light exposure suppresses melatonin, which may indirectly impair night-time retinal repair and antioxidant activity, adding to cumulative stress over years.
Functional-medicine perspective / what to emphasise
As part of blog: stress that eye health isn’t just optics—cellular health in retina matters (mitochondria, oxidative stress, peptides, etc.).
Early signs: frequent eye fatigue, need to squint or blink excessively, headaches after screen use, unexplained worsening of near/blur vision, dry/irritated eyes.
Modifiable factors: screen distance, lighting (glare, ambient), breaks (20-20-20 rule), outdoor (natural light) exposure for children/adults, consider blue‐light filter or lens, but emphasise that it’s supportiv,e not a substitute for behavioural change.
Nutritional support: antioxidants (lutein/zeaxanthin in macula), omega-3 (tear film health), mitochondrial support (CoQ10, ALA) may be useful adjuncts when you suspect cumulative damage.
💡 Functional Tip:
Follow the 20-20-20 rule — every 20 minutes, look 20 feet away for 20 seconds to relax eye muscles and reduce strain.
Support eye mitochondria and retinal antioxidant defences with these nutrients:
- Lutein & Zeaxanthin → dark leafy greens (spinach, kale, mustard greens), egg yolk, corn, orange & yellow peppers
- CoQ10 → fatty fish (sardines, mackerel), organ meats, peanuts, sesame seeds, whole grains
- Omega-3 fatty acids (DHA & EPA) → fatty fish (salmon, sardines), flaxseeds, chia seeds, walnuts
💡 Tip: Pair carotenoid-rich foods with healthy fats (ghee, olive oil, nuts) to improve absorption.

2. Sleep & Circadian Rhythm — Blue Light vs. Melatonin
That late-night scroll may feel relaxing, but your body reads it differently.
Screens, especially LED ones, emit blue-enriched light that tricks the brain into thinking it’s still daytime. This suppresses melatonin, the sleep hormone that helps you fall asleep and stay asleep.
According to research published in the Journal of Clinical Endocrinology & Metabolism, even 1–2 hours of evening screen exposure can delay melatonin release and shift your internal body clock. The result? Trouble sleeping, restless nights, groggy mornings, and daytime brain fog.
Mechanisms/implications
- Poor sleep interferes with many downstream systems: mitochondrial repair (many repair/mitochondrial biogenesis processes happen during deep sleep), hormonal regulation (growth hormone, cortisol rhythms), neurochemical resetting (glymphatic clearance in brain), peptide/hormone signalling (eg melatonin, orexin).
- Shifted circadian rhythm leads to misalignment between internal clock and external environment → reduced overall vitality, mood lability, increased risk of metabolic dysfunction (for example via disrupted cortisol/insulin rhythms).
- Screens just before bed = increased arousal (visual, cognitive, emotional) + delayed melatonin → cascade of poor sleep quality leading to daytime fatigue, brain fog, reduced mitochondrial efficiency.
Functional-medicine perspective
- Consider assessing sleep hygiene, device exposure windows (eg stop screens 60-90 min before bed), ambient lighting (warm light vs blue light), ensure sufficient dark period during night.
- Symptoms to watch: difficulty falling asleep, waking frequently at night, non-restorative sleep, morning grogginess, needing more sleep than you used to, daytime irritability or concentration problems.
Interventions:
- Establish fixed sleep-wake times, blackout curtains, red/amber evening light, screen filters/night mode, and device off in the bedroom. Support restoratively with melatonin (short-term, clinician supervision), magnesium at night, and mitochondrial/nutrient support to help repair (eg CoQ10 for mitochondrial support, antioxidant support).
💡 Functional Tip:
Avoid screens 1–2 hours before bed, or use blue-light filters and amber glasses. Support melatonin naturally with dark evenings, magnesium-rich foods, and exposure to morning sunlight.
3. Brain — Rewiring the Reward System
Our brains love novelty — and screens deliver it in endless supply. Each notification, like, or game win triggers a dopamine spike, the same chemical involved in motivation and addiction.
Over time, this overstimulation rewires our reward pathways, making us crave more screen time while real-world pleasures feel less satisfying.
MRI studies from Frontiers in Human Neuroscience reveal that excessive screen or gaming use can alter gray matter volume in brain regions linked to attention, impulse control, and emotional regulation. This helps explain why heavy users often struggle with focus, mood swings, or anxiety when offline.
Mechanisms/implications
- Screens (especially games/social media) give rapid feedback loops, variable reward/punishment, novelty — this can train the brain’s reward circuit (striatum, putamen) toward instant gratification, making slower tasks (reading, sustained effort) relatively less rewarding.
- Altered reward signaling can shift peptide/hormone/neurotransmitter balance (dopamine, endorphins, orexin, etc) → changes in craving, mood, attention.
- Structural brain changes: frontal control networks (executive function) may be under-stimulated or less developed in heavy users, especially in developing brains.
- Downstream effects: reduced focus, impaired learning and memory, greater emotional volatility, and impulsive behavior.
Functional-medicine perspective
- When working with clients: screen-use history (hours/day, type of content, device, time of day), look for signs of attention/learning issues, mood swings, craving/overuse behaviours.
- Early signs: needing shorter bursts of screen time before feeling bored, inability to focus on non-screen tasks, irritability when screen use is reduced, increased need for novelty.
Intervention:
- Digital-diet strategy: scheduled screen breaks, limit passive scrolling, prioritise slower, focused tasks, encourage “real-world” challenge tasks (reading, hands-on hobbies). Cognitive exercises for attention, mindfulness, reduce dopamine dependency.
- Nutritional/neurochemical support: ensure good omega-3 (brain membranes), B-vitamins (neurotransmitter synthesis), magnesium (calming), possibly L-theanine for focus, and lifestyle factors (physical exercise, nature exposure, novel tasks) to rebuild regulatory networks.
💡 Functional Tip:
Rebalance dopamine naturally through movement, sunlight, nature exposure, and deep work. Practice digital fasting — one day a week without screens to reset your brain’s chemistry.

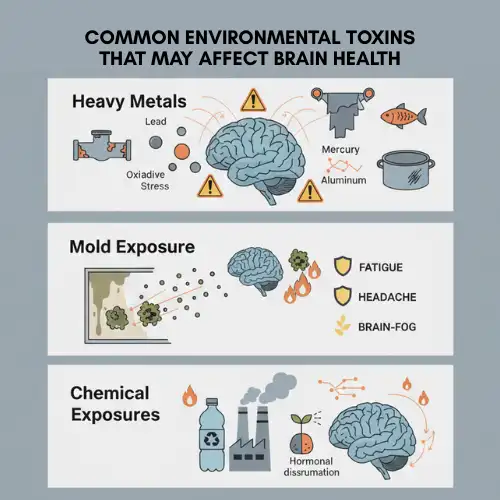
4. Mitochondria — The Hidden Energy Drain
Few people realize that screen habits affect us down to our cellular engines — the mitochondria.
Blue light and chronic sleep deprivation elevate oxidative stress, leading to mitochondrial dysfunction not just in the eyes, but throughout the body. A 2022 study in Redox Biology found that disrupted circadian rhythms directly impair mitochondrial energy production.
Mechanisms/implications
- Mitochondria are the energy generators of our cells. When they are stressed or damaged, the body produces less energy (ATP) and more oxidative stress, leading to cellular fatigue, faster ageing of cells, and impaired repair.
- In the context of screen use, repeated exposure to blue-heavy light may place stress on retinal cells—marked by poor sleep, reduced movement, and increased oxidative stress—can place strain on mitochondria throughout the body, indirectly affecting energy levels and blood-sugar balance over time.
- From a functional medicine perspective, poor mitochondrial health often shows up as persistent fatigue, slower recovery, reduced stress tolerance, mood changes, brain fog, insulin resistance, and stubborn weight gain.
Functional medicine perspective
During case history, it’s important to ask about:
- Daily screen time, especially evening and night-time use
- Exposure to bright or blue light from phones, laptops, and LEDs
- Sleep quality, sleep timing, and difficulty winding down
- Long periods of sitting or inactive screen use
- Symptoms such as ongoing fatigue, slow recovery after effort, brain fog, poor focus, and mental slowing
How this information is used:
- When available, specific tests related to cellular energy and oxidative stress may be reviewed.
- When testing is not practical, support can still begin by addressing the root contributors
Interventions:
- Blue-light reduction strategies (evening filters, screen-use limits)
- Nutrient support: CoQ10, alpha-lipoic acid, NAC, mitochondria-supportive diet (adequate protein, antioxidant-rich, omega-3, polyphenols)
- Movement and interval training to drive mitochondrial biogenesis (PGC-1α activation).
- Ensure sleep and circadian alignment because many mitochondrial repair processes happen in sleep and during dark/quiet periods.
💡 Functional Tip:
Feed your mitochondria with antioxidant-rich foods (berries, greens, turmeric), adequate sleep, and infrared light exposure (morning sunlight or red-light therapy).
5. Peptides & Hormonal Signalling — When Screens Confuse Your Chemistry
Your body’s hormones and brain messengers work best when daily rhythms are stable. Late-night screen use and constant digital stimulation disrupt these rhythms, altering melatonin (sleep), dopamine (reward), endorphins (calm), and insulin (blood sugar control).
Over time, this imbalance can lead to sleep disorders, anxiety or low mood, sugar cravings, weight gain, insulin resistance, prediabetes, PCOS, and burnout-related fatigue, along with reduced emotional resilience and energy.
Mechanisms / implications
- Disrupted melatonin → less synchronised circadian peptides/hormones → downstream metabolic dysregulation, mood disruption.
- Excessive reward stimulation (screens/games) → dopamine overshoot → down-regulation of dopamine receptors or shift in reward threshold → needing more stimulation, reduced pleasure from normal life → possible mood/anxiety issues.
- Metabolic peptides (insulin, leptin, ghrelin) get affected by poor sleep, sedentary behaviour, irregular eating which often accompany high screen-behaviour → risk of insulin resistance, weight gain.
- In functional-medicine terms: the brain/body signalling network is out-of-sync → fatigue, cravings, mood dysregulation, metabolic drift.
Functional-medicine perspective
- Assessment: ask about cravings, reward-seeking behaviour (screen/games/social media), mood swings, appetite/weight changes, sleep disruption, and attention issues.
- Make the link: Excess screen usage → reward/peptide stress → downstream metabolic & brain-health effects.
Interventions:
- Limit “high-stimulus” screen content (fast games, social media scrolling) and replace with slower, less dopamine-intense activities (reading, hands-on project, nature exposure).
- Support neurochemical resilience: omega-3s, B-vitamins, magnesium, adaptogens (if appropriate) for HPA-axis / neuro-modulation.
Reinforce natural reward systems: exercise, nature, creativity, and social real-life interaction. - Stabilise sleep/circadian system (see above) so peptides/hormones synchronise properly.
💡 Functional Tip:
Eat meals at regular times, prioritize protein and omega-3 fats, and practice mindful screen use — especially during meals or before sleep — to keep your body’s peptides and hormones in sync.
6. Whole-Body Effects — From Sedentary Screens to Stressed Systems
Screens often mean sitting, and sitting means stagnation.
The more time we spend online, the less we move, which affects our metabolism, lymphatic flow, and mood regulation.
Research in The Lancet Psychiatry found a strong link between screen time and depression, especially in teens and young adults. Prolonged inactivity also leads to insulin resistance, weight gain, and poor circulation — key drivers of inflammation and chronic disease.
Mechanisms/implications
Sedentary screen time → low physical activity → lower mitochondrial biogenesis, fewer muscle contractions (muscle is a metabolic organ) → reduced metabolic capacity.
Poor sleep + circadian misalignment (see above) → dysregulated cortisol, insulin, leptin/ghrelin → metabolic drift.
Brain reward dysregulation + mood impact → can lead to emotional eating, comfort-snacking, sedentary mood states.
Inflammatory milieu: increased sedentary time + poor sleep + high screen load may increase chronic low-grade inflammation, which burdens mitochondria and peptides.
Functional-medicine perspective
Assessment: screen-time minutes/day, physical activity minutes/day, sitting time, number of breaks, mood/stress levels, weight/waist changes, lab markers (glucose, insulin, lipids, inflammatory markers).
Interventions:
- Break up sedentary time: every 30-45 minutes, get up, move/stretch, use “active screen breaks”.
- Incorporate resistance + aerobic exercise to boost mitochondrial and metabolic health.
- Monitor metabolic markers regularly (fasting insulin, HOMA-IR, HbA1c, lipids).
- Address mood/stress: implement mindfulness, social interaction, real-life engagement rather than passive screen absorption.
- Diet: focus on whole foods, high antioxidant load, moderate glycemic load to mitigate the metabolic burden.
💡 Functional Tip:
Set movement reminders every hour. Try “habit stacking” — do squats while watching reels or stretch during a call. Reconnect your body to motion.
Functional Medicine View: Restoring Digital Balance
Functional medicine doesn’t tell you to throw away your phone — it helps you create harmony between technology and biology.
Here’s how you can start:
- Detox your circadian rhythm: Prioritize morning sunlight and dim evening lights.
- Nourish your cells: Eat anti-inflammatory, mitochondria-supportive foods.
- Support your nervous system: Use adaptogens like ashwagandha or rhodiola, and practice digital mindfulness.
- Rebuild real connections: Engage in activities that activate oxytocin — eye contact, laughter, shared meals, nature time.
Frequently Asked Questions (FAQs)
1. Is screen time actually damaging my health, or is it just causing temporary discomfort?
Screen use itself isn’t inherently harmful, but how and when we use screens matters. Occasional eye strain or late nights may feel temporary, but chronic overexposure—especially at night—can disrupt sleep, stress mitochondria, alter brain reward pathways, and impair metabolic and hormonal balance over time. The impact is cumulative, not immediate, which is why many people don’t connect their fatigue, brain fog, or mood changes to screen habits until years later.
2. Do blue-light filters and glasses fully protect me from screen-related problems?
Blue-light filters and glasses can reduce glare and ease eye strain, but they are supportive tools—not complete solutions. They don’t address reduced blinking, prolonged near-focus, dopamine overstimulation, sedentary behavior, or circadian disruption caused by late-night screen use. Behavioral changes, such as screen breaks, earlier device cut-off times, outdoor light exposure, and movement, remain the most effective interventions.
3. Can excessive screen use really affect energy levels, weight, and hormones?
Yes. Screen overuse often leads to poor sleep, reduced physical activity, and disrupted circadian rhythms—all of which influence insulin, cortisol, melatonin, leptin, and dopamine signaling. Over time, this can contribute to low energy, increased cravings, weight gain, insulin resistance, mood changes, and burnout. From a functional-medicine perspective, these issues stem from disrupted biological signaling rather than willpower alone.
4. What’s the most realistic way to reduce screen damage without giving up technology?
The goal isn’t digital elimination—it’s digital alignment. Start by switching off screens 60–90 minutes before bed to protect melatonin and sleep quality, and get morning sunlight to reset your circadian rhythm. Take regular movement breaks during screen use to counter sedentary strain, and consciously limit high-dopamine activities like endless scrolling or gaming that overstimulate the brain. Support your body from the inside with antioxidant-rich foods, omega-3 fats, and consistent, high-quality sleep. These small, sustainable changes work with your biology and restore balance far more effectively than extreme digital detoxes.
Conclusion: Entertainment at the Cost of Energy
The irony is clear — the tools designed to entertain and connect us are slowly disconnecting us from our biology.
When entertainment turns into dependency, our eyes strain, our sleep fades, our brain rewires, and our cells lose energy.
But awarenehttps://hormonereset.in/contact-us/ss is power. By blending modern technology with ancient biological wisdom — light, rest, movement, connection — we can reclaim the balance that our bodies are quietly craving.
Because true entertainment isn’t what numbs you — it’s what nourishes your energy and lights up your life.

References
- The influence of blue light on sleep, performance and wellbeing in young adults: A systematic review- National Library of Medicine
- Digital Screen Time and Myopia: A Systematic Review and Dose-Response Meta-Analysis– National Library of Medicine
- The association between screen time exposure and myopia in children and adolescents– Springer Nature Link
- Modeling the influence of nighttime light on melatonin suppression in humans -ScienceDirect
- The adverse impact of excessive smartphone screen-time on sleep quality among young adults– National Library of Medicine
- Comparative Effects of Red and Blue LED Light on Melatonin Levels During Three-Hour Exposure in Healthy Adults– MDPI
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset