Table of Contents
In a world obsessed with imported “superfoods,” one of the most potent metabolic foods has been hiding in plain sight for thousands of years: Horse gram. Known as Kulthi in Ayurveda and Kollu in South India, this humble legume is making a comeback—not just as food, but as functional medicine. Its unique nutrient profile and bioactive compounds offer benefits for glucose balance, gut health, hormone metabolism, and inflammation.

What is Horse Gram?
Horse gram (Macrotyloma uniflorum) is a drought-resistant legume traditionally consumed across India, Sri Lanka, and Southeast Asia. Historically, it was fed to warriors and livestock for endurance and strength, and was valued for its therapeutic properties in traditional medical systems.
Ancient History & Traditional Use
In Ayurvedic texts like Charaka Samhita, horse gram is described as a food that balances doshas, especially Kapha and Vata, and supports digestion. Siddha and folk traditions have used it for conditions like kidney stones (Mutrashmari), obesity (Medoroga), and poor digestion—long before modern science began exploring its medicinal potential. Its heating nature was traditionally prized for activating metabolism and clearing internal toxins.
Nutritional Powerhouse with Functional Potential
Horse gram stands out among pulses for its:
- High-quality plant protein, amongst the highest in the plant kingdom
- Very high dietary fiber, supporting gut and metabolic health
- Rich polyphenols and antioxidants, helping reduce inflammation
- Naturally low glycemic impact, beneficial for blood-sugar balance
- High iron content, supporting energy levels and hemoglobin
- Good calcium content, supporting bone and metabolic function
In traditional systems, horse gram is also considered high-pranic—a food believed to enhance vital energy, warmth, and metabolic fire, making it especially valuable for sedentary, cold, or sluggish metabolic states.
From an Ayurvedic perspective, it (Kulthi) is considered ushna (warming), ruksha (dry), and tikshna (penetrating). It is traditionally used to stimulate agni (digestive fire), reduce kapha accumulation, and clear ama (metabolic waste). Because of its high pranic value, it is believed to enhance vital energy, circulation, and metabolic strength, making it especially beneficial for sluggish digestion, fluid retention, and cold, sedentary body types.
Scientifically Documented Benefits
1. Anti-Inflammatory & Antioxidant Effects
Research shows that horse gram can boost antioxidant enzyme activities like superoxide dismutase and catalase, potentially helping reduce oxidative stress and inflammation in the body. In animal models, horse gram supplementation increased antioxidant status without activating pro-inflammatory mediators.
Studies have shown that the oil extracted from horse gram seeds—referred to in research as its fixed oil—contains bioactive fatty acids and plant compounds with pain-relieving and anti-inflammatory properties. Unlike essential oils, fixed oils are stable, non-volatile oils that support cell membrane health and help regulate inflammatory pathways in the body. These findings provide a scientific explanation for horse gram’s traditional use in easing joint pain, muscle aches, and other inflammatory conditions, bridging ancient dietary wisdom with modern nutritional science.
2. Metabolic Health: Glucose & Lipid Regulation
While large human clinical trials are still limited, animal studies and systematic reviews suggest that horse gram may act as an antidiabetic and lipid-modulating food. Its bioactive compounds—including polyphenols, resistant starch, and dietary fibre—appear to influence glucose metabolism, improve insulin sensitivity, and favourably modify lipid parameters such as total cholesterol, LDL cholesterol, triglycerides, and the LDL:HDL ratio. Some studies also note improvements in oxidative stress and inflammatory markers, which are central to cardiometabolic risk. These effects are particularly relevant for modern lifestyle conditions such as PCOS, insulin resistance, metabolic syndrome, fatty liver disease, and cardiovascular disease (CVD) risk.
Fermented horse gram products have also shown inhibition of enzymes related to fat digestion, indicating potential anti-obesity effects.
3. Kidney Protection & Diuretic Action
Traditional use of horse gram for urinary health is supported by studies showing diuretic activity and protective effects in nephrotoxicity models. These findings align with its historical use in preventing or managing kidney stones and supporting overall kidney function.
4. Antioxidants & Phytochemicals
The seeds are rich in phenolics, flavonoids, and tannins, which contribute to its antioxidant, antimicrobial, and potential therapeutic properties. These compounds are linked to a range of physiological effects from gut health support to reduced oxidative damage.
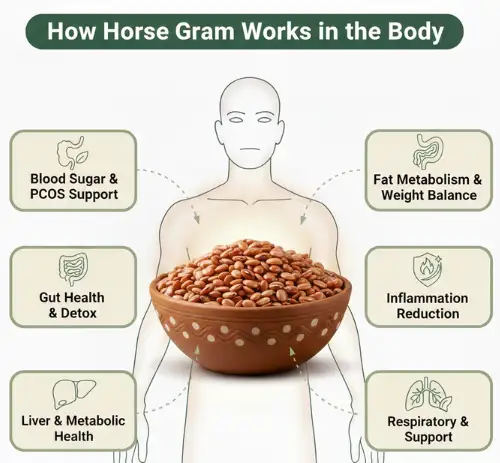
Functional Medicine Perspective: How Horse Gram Works in the Body
Blood Sugar Regulation & PCOS
The high fiber and polyphenol content slow carbohydrate absorption, helping stabilize glucose levels—which is vital if you’re managing insulin resistance, PCOS, or metabolic syndrome.
Gut Health & Detoxification
Fiber supports bowel regularity and gut microbiome health. A healthier gut means improved hormone metabolism and reduced systemic inflammation.
Fat Metabolism & Weight Management
Traditional sources consider horse gram deepana (digestive fire enhancer). Modern studies support effects on fat digestion and enzyme activity, helping with satiety and metabolic efficiency.
Inflammation Modulation
The antioxidants and anti-inflammatory compounds in horse gram help the body neutralize harmful free radicals and reduce chronic inflammation in tissues. For patients, this can translate into:
- Reduced fatigue and improved energy, as cells are less stressed and can produce energy more efficiently
- Better metabolic health, including improved blood sugar control and lipid balance
- Support for liver function, helping reduce fat accumulation in conditions like fatty liver
- Joint and muscle comfort, as inflammation in connective tissues decreases
- Enhanced cardiovascular health by lowering oxidative stress and improving blood vessel function
In short, these compounds help the body recover, repair, and function optimally, making horse gram a supportive food for conditions like insulin resistance, PCOS, fatty liver, and mild inflammatory states.
Support respiratory health
Horse gram has traditionally been used in Ayurveda to support respiratory health and help relieve cold, cough, and congestion. Its warming, drying, and anti-inflammatory properties can help soothe the respiratory tract, reduce mucus buildup, and ease irritation in the throat and lungs. Additionally, the antioxidants and bioactive compounds may support the immune system, helping the body respond better to infections or seasonal colds, making it a gentle, food-based way to support overall respiratory wellness.
Who Should Use Caution?
Despite its benefits, horse gram is heating and high in fiber, which may be intense for some individuals.
Avoid or consume cautiously if you have:
- Active gastritis or ulcers
- Thyroid conditions without proper soaking & preparation
- Pregnancy or sensitive digestion (without guidance)
How to Prepare Horse Gram Correctly (Essential Step)
Proper preparation reduces phytic acid and gas-forming compounds, enhances digestibility, and unlocks therapeutic benefits.
Soaking + Spicing Protocol:
- Soak 10–12 hours
- Discard soaking water
- Pressure-cook thoroughly
- Add digestive spices:
Ginger, cumin, asafoetida (hing), curry leaves
This simple method enhances bioavailability and reduces digestive strain.
Gluten-Free, Sugar-Free & Dairy-Free Horse Gram Recipes
1. Horse Gram Rasam — Detox & Gut Support
A light, tangy broth with cooked horse gram water, spices, and herbs—ideal on bloating or fatty liver days.
2. Horse Gram Chutney Powder — PCOS-Friendly Condiment
Roasted horse gram + sesame + curry leaves make a fiber-rich, nutrient-dense topping for millets.
3. Horse Gram Soup — Reset Meal
Blend cooked horse gram with ginger, turmeric, and seasonal veggies for a metabolic reset.
4. Sprouted Horse Gram Sundal — High-Protein Snack
Sprouted and lightly tempered with mustard seeds and lemon—a perfect plant-based protein snack.
Best Time & Frequency to Consume
- 1–2 times per week is sufficient for most
- Best during winter & monsoon
- Ideal at lunch (strongest digestion)
Frequently Asked Questions (FAQs)
1. Is horse gram safe to consume regularly?
It is safe for most people when consumed in moderation and properly prepared. Because it is high in fiber and warming in nature, it is best eaten 1–2 times per week, especially during cooler seasons. Proper soaking, thorough cooking, and the use of digestive spices improve tolerance and reduce digestive discomfort.
2. Can horse gram help with PCOS and insulin resistance?
It may support metabolic health due to its high fiber content, low glycaemic impact, and polyphenols, which help stabilize blood sugar and improve insulin sensitivity. While it is not a treatment for PCOS, it can be a supportive food as part of a balanced, root-cause-based nutrition plan.
3. Does horse gram support gut health?
Yes. The dietary fiber in horse gram supports bowel regularity and gut microbiome balance, which are important for hormone metabolism and inflammation control. A healthier gut can help the body process and eliminate hormones more efficiently, supporting overall metabolic and hormonal balance.
4. Who should avoid or limit horse gram?
It should be consumed cautiously by individuals with active gastritis, ulcers, very sensitive digestion, pregnancy, or thyroid conditions if not properly prepared. In such cases, it’s best to seek guidance from a qualified healthcare or Functional Medicine practitioner before including it regularly.
Closing Thoughts: Ancient Wisdom Meets Modern Science
Horse gram is a classic functional food—one that not only nourishes but also actively supports the body’s healing and metabolic systems. Packed with high-quality protein, dietary fiber, polyphenols, antioxidants, iron, and calcium, it helps improve blood sugar control, lipid balance, gut health, and energy metabolism. Its anti-inflammatory and antioxidant properties support tissue repair, reduce oxidative stress, and may help manage conditions such as PCOS, insulin resistance, fatty liver, cardiovascular risk, and mild inflammatory states. Traditionally valued for its warming and pranic qualities, horse gram also supports digestion, immunity, and even respiratory health, helping with cold and cough.
In bridging ancient wisdom and modern science, horse gram reminds us that sometimes the oldest foods are the most healing, offering both nourishment and therapeutic benefit in today’s modern lifestyle.

References
- Nutritional Profile and Therapeutic Properties of Horse Gram– Open Science Publications.
- Traditional uses, phytochemistry, pharmacology, and nutraceutical potential of horse gram– National Library of Medicine
- Kaulath, a new fermented food from horse gram– National Library of Medicine
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset