Table of Contents
Hormones are the silent conductors of your body’s symphony—regulating energy, metabolism, mood, reproduction, and immunity. When they’re out of balance, even simple daily tasks can feel exhausting. But hormonal imbalance is rarely a standalone problem—it’s usually a signal that something deeper in your body’s communication system is off.
At Hormone Reset, our approach goes beyond masking symptoms. We focus on identifying the root causes—from stress and gut health to thyroid dysfunction and environmental toxins—so you can rebalance your system naturally and sustainably.

1. Stress and Cortisol Imbalance: How Chronic Stress Disrupts Hormones
Chronic stress doesn’t just make you anxious—it rewires your hormonal network. The HPA (hypothalamic-pituitary-adrenal) axis controls cortisol, the stress hormone, which directly affects thyroid conversion, insulin regulation, estrogen metabolism, and reproductive hormones.
How stress disrupts hormones:
- Cortisol overload: Persistent stress initially elevates cortisol, suppressing thyroid hormone conversion (T4 → T3) and leading to fatigue, brain fog, and low metabolism.
- Adrenal burnout: Over time, some people experience low cortisol, contributing to chronic fatigue, mood swings, and blood sugar instability.
- Estrogen and progesterone imbalance: Stress promotes estrogen dominance, worsening PMS, thyroid dysfunction, and fat retention.
- Insulin spikes: Elevated cortisol increases blood sugar, fueling inflammation and worsening autoimmune conditions like Hashimoto’s.
How Hormone Reset helps:
- Mindfulness and meditation to retrain the stress response.
- Adaptogens like ashwagandha and rhodiola for adrenal support.
- Targeted nutrition to stabilize cortisol and support adrenal function.
- Lifestyle adjustments, including structured sleep, work-life balance, and gentle exercise.
2. Gut Health: The Hidden Driver of Hormone Imbalance
Did you know 70–80% of your immune system resides in your gut? A compromised gut lining, dysbiosis, or small intestinal bacterial overgrowth (SIBO) can trigger autoimmune attacks on the thyroid, disrupt estrogen metabolism, and affect serotonin production—leading to fatigue, mood swings, and thyroid dysfunction.
Mechanisms at play:
- Leaky gut: Toxins enter the bloodstream, causing immune confusion and potentially attacking thyroid tissue (Hashimoto’s) or other endocrine organs.
- Microbiome imbalance: Disrupted gut flora impairs hormone metabolism, including estrogen reabsorption and thyroid conversion.
- Chronic inflammation: Promotes insulin resistance, worsens autoimmune reactions, and fuels hormone disruption.
Hormone Reset interventions:
- Gut-healing nutrition: collagen, bone broth, L-glutamine, and zinc.
- Fermented foods and high-quality probiotics for microbiome balance.
- An anti-inflammatory, nutrient-dense diet eliminating gluten, dairy, refined sugar, and additives.
- Toxin reduction: organic produce, filtered water, and avoiding processed products.
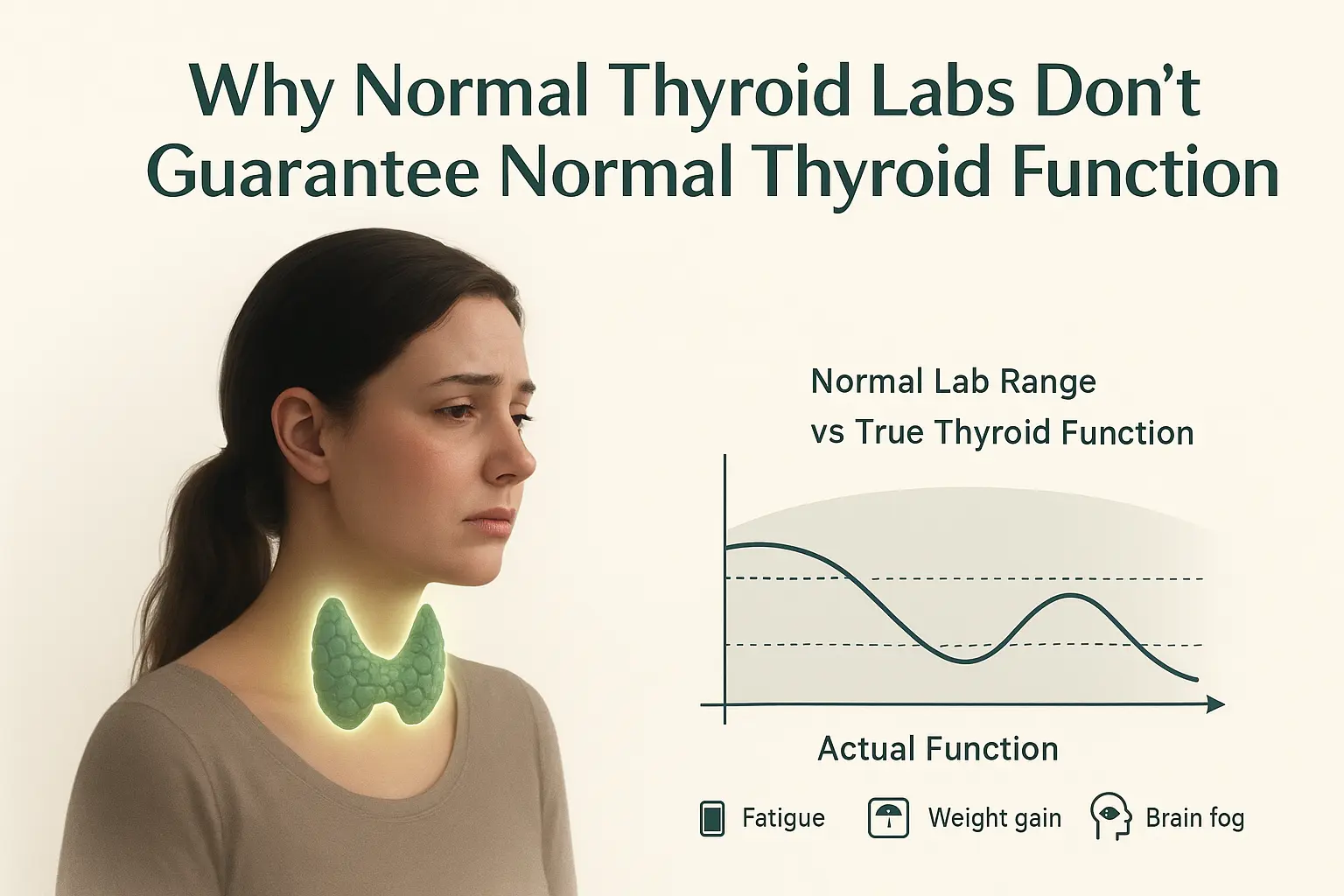
3. Thyroid Dysfunction: Root Cause, Not Just Symptoms
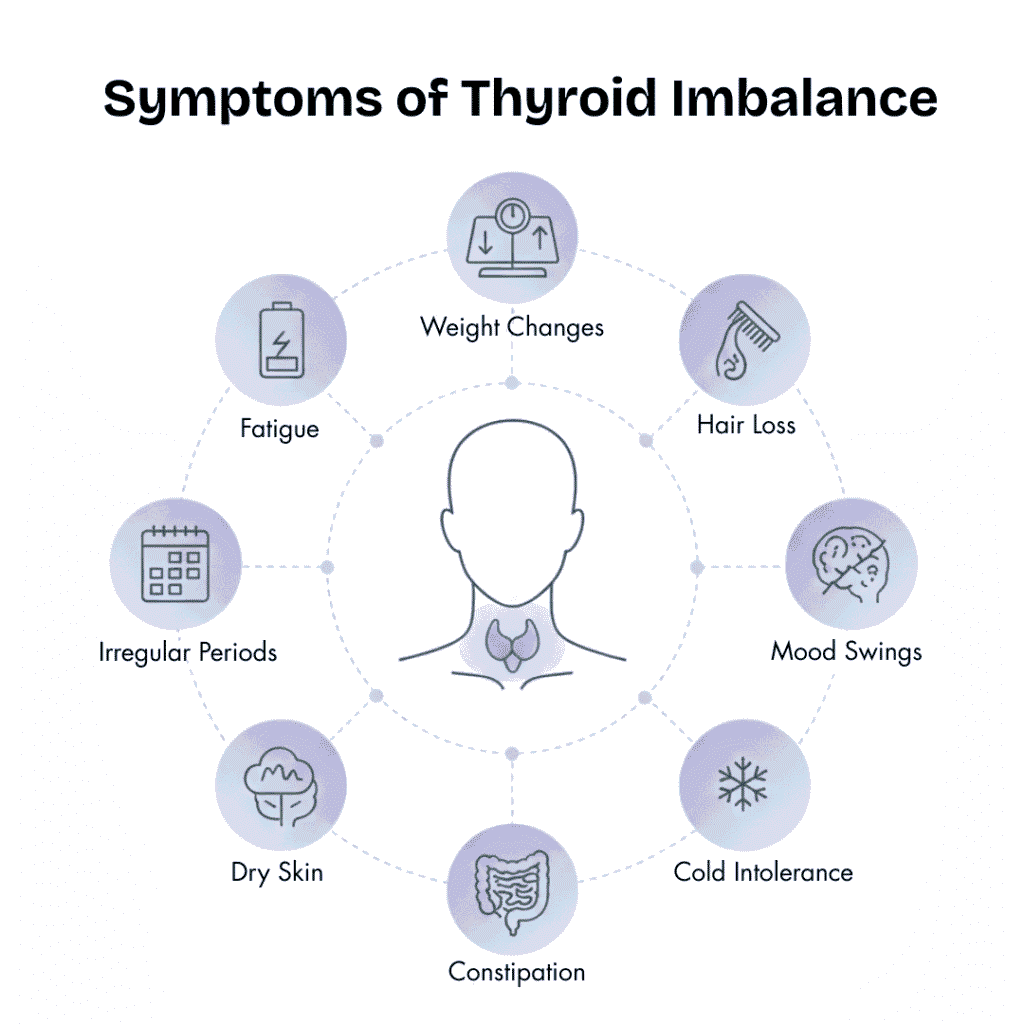
Thyroid imbalances are often misunderstood. Conditions like Hashimoto’s thyroiditis or hypothyroidism affect metabolism, mood, energy, and reproductive hormones—but are rarely isolated problems. At Hormone Reset, we focus on why the thyroid is under attack or underperforming, not just hormone replacement.
Root causes include:
- Autoimmune triggers linked to gut inflammation and molecular mimicry.
- Nutrient deficiencies (selenium, zinc, iodine, and vitamin D) prevent optimal hormone production.
- Impaired liver detoxification reduces T4 → T3 conversion.
- Chronic stress elevates cortisol, suppressing thyroid output.
Hormone Reset approach:
- Personalized nutrition: support thyroid hormone synthesis and balance estrogen, progesterone, and insulin.
- Targeted supplementation: high-potency nutrients when diet alone isn’t sufficient.
- Lifestyle adjustments: stress management, sleep optimization, and gentle physical activity.
- Detox support: liver-focused interventions to optimize hormone metabolism.

4. Nutritional Deficiencies: Fueling Hormonal Health
Hormone production depends on specific nutrients. Deficiencies not only reduce hormone synthesis but can amplify autoimmune and metabolic dysfunction.
Critical nutrients:
- Selenium & Zinc: Protect thyroid cells, support adrenal function, and reduce oxidative stress.
- Iodine: Essential for T3 and T4 thyroid hormones (must be carefully monitored in Hashimoto’s).
- Vitamin D: Regulates immunity and reduces autoimmune flares.
- Omega-3 fatty acids: Reduce inflammation and improve cell membrane function.
- Magnesium & B vitamins: Support energy production, neurotransmitter balance, and stress resilience.
Hormone Reset strategies:
- Dietary optimization using nutrient-dense foods.
- High-quality, clinically-tested supplements where needed.
- Integration with lifestyle practices for absorption and utilization.
5. Environmental Toxins: Invisible Disruptors of Hormones
Endocrine-disrupting chemicals (EDCs) like BPA, phthalates, pesticides, and personal care chemicals mimic or block hormones, interfering with estrogen, testosterone, and thyroid signaling.
Impact on hormone metabolism:
- Estrogen dominance from xenoestrogens.
- Thyroid receptor interference.
- Impaired detoxification leading to the accumulation of hormone-disrupting compounds.
Functional strategies:
- Use glass or stainless steel containers instead of plastic.
- Choose organic foods when possible.
- Opt for clean, non-toxic personal care products.
- Support liver detoxification pathways with cruciferous vegetables and hydration.
6. Women’s Hormonal Issues: PCOS, PMS, Endometriosis
Female-specific conditions often amplify systemic hormone imbalances. Insulin resistance, estrogen dominance, and inflammation interconnect with thyroid and adrenal function.
Hormone Reset interventions:
- Diet and lifestyle modifications to manage insulin and inflammation.
- Personalized hormone-balancing protocols integrating stress, sleep, and gut health.
- Targeted nutrition to stabilize estrogen and progesterone levels.
- Symptom tracking and iterative program adjustments.
7. Sleep & Circadian Rhythm: Timing Is Everything
Sleep is a critical hormone regulator. Disrupted circadian rhythm elevates cortisol, impairs melatonin production, and affects insulin, thyroid, and reproductive hormones.
Hormone Reset recommendations:
- Maintain consistent sleep and wake times.
- Avoid screens and blue light 1–2 hours before bed.
- Optimize bedroom environment: darkness, cool temperature, minimal noise.
- Support circadian alignment with morning sunlight exposure.
8. Lifestyle & Physical Activity: Balance Is Key
Both inactivity and overtraining disrupt hormone networks.
- Sedentary lifestyle → lowers metabolism, increases cortisol, promotes insulin resistance.
- Excessive or irregular training → adrenal stress, inflammation, and impaired thyroid conversion.
Hormone Reset approach:
- Moderate, consistent physical activity (walking, yoga, strength training).
- Balance exercise with recovery to prevent adrenal burnout.
- Integrate stress management and nutrition to support activity-induced hormone adaptation.
Conclusion: Addressing Root Causes, Not Just Symptoms
Our personalized programs guide you step by step, combining functional medicine, targeted nutrition, stress management, gut healing, and lifestyle optimization to bring your hormones back into balance—naturally, sustainably, and effectively.
Hormonal imbalance is rarely an isolated issue. By understanding and addressing the root causes—stress, gut health, thyroid dysfunction, nutrient deficiencies, environmental toxins, and lifestyle factors—Hormone Reset helps restore your body’s hormonal symphony.
FAQs: Hormone Reset and Hormonal Health
1. What causes hormonal imbalance in women and men?
Hormonal imbalance can arise from multiple factors, including chronic stress, poor gut health, thyroid dysfunction, nutrient deficiencies, environmental toxins, and lifestyle issues such as sleep disruption or irregular physical activity. These factors interfere with your body’s endocrine network, leading to fatigue, mood swings, metabolic changes, and reproductive health issues.
2. How does stress affect hormones?
Chronic stress disrupts the HPA axis, elevating cortisol levels. High cortisol can suppress thyroid hormone conversion (T4 → T3), promote insulin spikes, and create estrogen dominance, contributing to fatigue, brain fog, PMS, and weight gain. Over time, adrenal burnout may occur, resulting in low cortisol and chronic fatigue.
3. Can gut health impact my hormone levels?
Absolutely. Around 70–80% of the immune system resides in the gut. Gut imbalances, leaky gut, or dysbiosis can trigger autoimmune responses, impair estrogen metabolism, disrupt thyroid function, and affect neurotransmitter production, causing fatigue, mood swings, and other hormonal issues. Healing the gut is critical for overall hormonal balance.
5. Are thyroid problems the root cause or just a symptom?
Thyroid dysfunction is often a symptom of underlying issues such as autoimmune attacks (e.g., Hashimoto’s), nutrient deficiencies (selenium, zinc, iodine), liver detox issues, or chronic stress. Addressing the root causes, rather than only taking hormone replacement, leads to sustainable improvement in energy, metabolism, and overall hormonal health
6. How does Hormone Reset personalize treatment for lasting results?
Hormone Reset takes a holistic, root-cause approach. Programs combine stress management, gut healing, nutrition optimization, targeted supplementation, detox support, and lifestyle adjustments. This integrative method addresses your specific hormonal imbalances and works to restore long-term balance naturally and sustainably.
References
Integrative Overview of Hypothyroidism:
Holistic Understanding of Hypothyroidism & Root-Cause Evaluation –Caring for the Body
Functional Medicine Approach to Thyroid & Hormone Health:
Comprehensive Hormone and Thyroid Wellness Strategies –Modern Holistic Health
Integrative Medicine for Thyroid Hormone Imbalance:
How Integrative Medicine Supports Thyroid Hormone Balance –Mindfully Integrative
Evidence-Based Thyroid Functional Medicine Framework:
Balancing Thyroid Hormones Naturally: Clinical Insights –Institute for Functional Medicine (IFM)
Gut–Thyroid Axis Research:
Understanding the Gut–Thyroid Connection in Hypothyroidism –Walsh Approach
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset
o