Table of Contents
In India today, an increasing number of people are waiting months—or even years—for relief from autoimmune conditions such as Hashimoto’s thyroiditis, Rheumatoid arthritis, Psoriasis, or Lupus. Many feel trapped in symptom-management loops: the medication helps, the flare-ups return, fatigue lingers, and labs bounce. But what if the answer wasn’t just managing the immune attack—but rewinding it? That’s the promise of functional medicine. In this article, we dive into how functional medicine in India is being used to go beyond surface care and build a 90-day healing strategy for autoimmune symptoms.
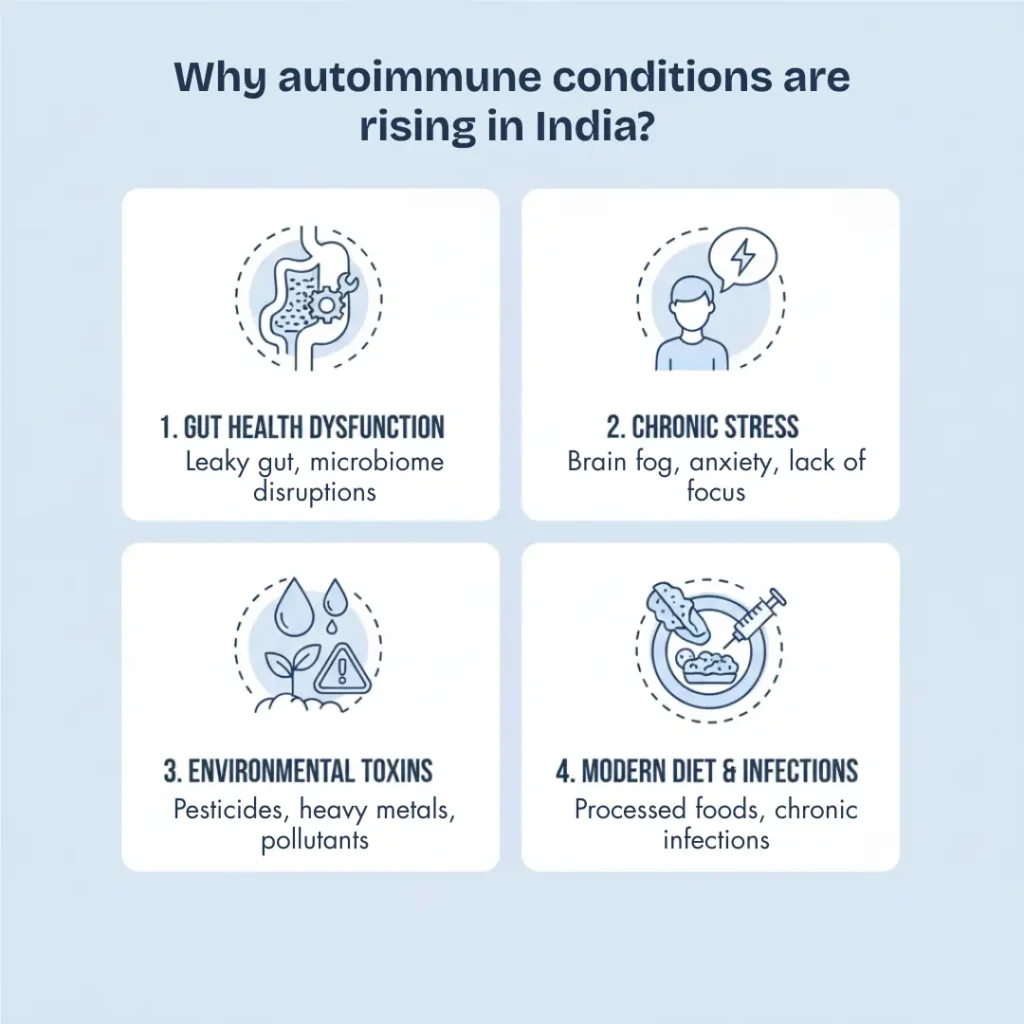
Why Autoimmune Conditions Are Rising in India
India is navigating a complex health scenario: while infectious diseases still demand attention, non-communicable and immune-mediated disorders are surging. For example, recent reporting indicates that nearly 70% of autoimmune disease patients in India are women, due to hormonal, environmental, and lifestyle factors. The Times of India
Meanwhile, a 2021 panel of experts noted that functional medicine may help reverse chronic and autoimmune diseases by addressing root causes rather than simply suppressing symptoms. ETHealthworld.com
Key drivers in India include:
- Urbanisation and sedentary behaviours
- A well-balanced traditional diet is turning into processed food loaded with refined carbohydrates and trans fats, etc.
- Environmental toxicity, air and indoor pollution (impacting the immune and respiratory systems)
- Delayed diagnosis or fragmented care in autoimmune cases
- Stress, poor sleep, chronic infections, and gut dysbiosis (often unaddressed)
In such a backdrop, functional medicine—which emphasises root-cause discovery and personalised protocols—is increasingly relevant for autoimmune health.
What is Functional Medicine — A Root-Cause Approach
Functional medicine is a systems-based, patient-centred model that seeks to identify why the body is mis-regulating, rather than only what is mis-regulating. It is especially relevant for complex conditions like autoimmunity, where multiple systems (gut, hormones, inflammation, immune regulation) interact.
In India, functional medicine clinics emphasise: personalised history + advanced lab testing + tailored nutrition + lifestyle optimisation + targeted root cause solutions. For example, Indian clinics describe root causes as gut-health imbalance, toxin exposure, chronic infections, and hormonal disruption.
Unlike conventional medicine that might prescribe immunosuppressants or symptomatic relief, functional medicine asks:
- What triggered the immune system to misfire?
- Which body systems are exhausted or overloaded?
- What lifestyle or environmental exposures keep the inflammation active?
Thus, the function-medicine approach can often complement conventional treatment and, over time, reduce flare-ups, medication dependency, and improve life quality.
Discover how our clients transformed their health with Hormone Reset. Read their success stories!
The 90-Day Healing Framework: What It Typically Includes
While every individual is unique, a structured 90-day framework gives a realistic timeline for meaningful improvement in autoimmune symptoms. Here’s a typical blueprint:
Days 1-30: Stabilise & Reset
- Comprehensive assessment: full history, gut/hormone/immune labs
- Elimination or anti-inflammatory nutrition plan (e.g., whole foods, reduced gluten/processed sugar)
- Gut health: identify and address issues and imbalances related to stomach acid production, enzyme output, imbalances and overgrowths of bacteria, fungus and parasites in the gut, and heal the gut lining with probiotics, prebiotics, nutrients like zinc or L-glutamine, etc
- Detoxify and reduce environmental triggers (pollution exposure, indoor smoke, toxins)
- Begin supportive lifestyle changes: consistent sleep, stress reduction (meditation or yoga)
Days 31-60: Rebuild Systems
- Reintroduce nutrient-dense foods adapted to the Indian diet (e.g., legumes, regional vegetables, healthy fats)
- Hormone optimisation: adrenal/thyroid support if needed
- Detoxification support: liver/gut/lifestyle practice
- Moderate exercise and movement to support immune regulation
- Monitor labs and symptoms to adapt the plan
Days 61-90: Reinforce & Integrate
- Immune retraining: focus on balance, not suppression (e.g., micronutrients like vitamin D, omega-3, curcumin)
- Full integration of lifestyle: stress management, sleep hygiene, movement rhythm
- Transition to sustainable habits rather than a “temporary fix”
- Reassess labs and symptoms: aim to reduce flare-ups, stabilise immune markers, improve quality of life
This 90-day timeframe is not a “cure guarantee”, but most patients report meaningful symptom reduction, fewer flares, and greater energy in this period. Clinics in India emphasise root-cause treatment over quick fixes.
Key Root-Cause Factors That Functional Medicine Targets
Understanding what triggers the “autoimmune misfire” is key. Functional medicine often focuses on:
Gut Health & Microbiome
Overgrowth of the microbial/fungal/parasitic populations in the gut leads to higher gut toxicity and resultant immune system overactivation. This often leads to a compromised gut barrier (“leaky gut”), which in turn allows undigested food molecules and toxins into the bloodstream, triggering further immune dysregulation. Functional medicine emphasises gut healing via diet, targeted supplements, herbs, probiotics, and lifestyle.
Toxin Load & Environment
In India, heavy metal exposure, industrial pollutants, indoor air pollution, and chronic toxin load contribute to immune stress. Functional medicine aims to remove or reduce these exposures and support detox pathways. ETHealthworld.com
Nutrient & Hormone Imbalances
Vitamin D deficiency, omega-3 shortfall, thyroid/adrenal stress, and hormone imbalance all affect immune regulation. For example, research shows lower levels of vitamin D is linked with increased autoimmunity. arXiv
Chronic Stress & Sleep Disturbance
Chronic psychological stress elevates cortisol, dysregulates immunity, and triggers flares. The positive impact of mind-body practices like yoga for autoimmune disorders has been documented in India and globally. PubMed
What Results Can You Realistically Expect in 90 Days?
Let’s set realistic expectations:
- Significant Symptom reduction: fewer flare-ups, less fatigue, better mood, and sleep
- Improved lab markers: reduced inflammation (CRP), stabilised thyroid/hormone values, better gut health parameters
- Reduced medication dependency: under supervision, some patients manage to reduce flare-prevention doses
- Empowerment and sustainable habits: shift in diet, stress, lifestyle that supports long-term wellness
Importantly, “reverse” does not always mean disease extinction, but rather “long-term remission”, improved quality of life and root-cause control. Indian reports suggest functional-medicine practitioners believe many chronic/autoimmune issues can be reversed if the root causes are identified and addressed. ETHealthworld.com
Choosing the Right Functional Medicine Practitioner in India
If you decide to pursue this route, here is a checklist:
- Certified training in functional/integrative medicine (and experience in autoimmune cases)
- Uses advanced diagnostics (gut, hormone, toxins), not just standard labs
- Offers personalised nutrition, lifestyle + environmental support—not just supplements
- Transparent about costs, time frame, and realistic outcomes
- Encourages collaboration with your conventional medical provider (especially for medications)
Frequently Asked Questions About Functional Medicine for Autoimmune Healing
Can Functional Medicine Really Help Improve Autoimmune Conditions?
Functional medicine does not promise a cure, but it helps many people experience significant relief by addressing the underlying triggers of autoimmunity. Instead of only controlling flare-ups, this approach works on improving gut health, reducing inflammation, balancing hormones, and calming an overactive immune system. As these root causes are addressed, most individuals begin noticing fewer symptoms and better energy within the first 90 days.
How Is Functional Medicine Different From Conventional Treatment?
Conventional care often focuses on symptom control through medications that suppress the immune response. Functional medicine, on the other hand, asks why the immune system is misfiring in the first place. By identifying factors such as nutrient deficiencies, environmental toxins, gut imbalance, stress, and hidden inflammation, it builds a personalised plan that restores balance rather than masking symptoms.
What Conditions Can Benefit From a Functional Medicine Approach?
Many autoimmune conditions—such as Hashimoto’s thyroiditis, Rheumatoid arthritis, Psoriasis, Lupus, and IBD—respond well to a root-cause strategy. People dealing with chronic fatigue, digestive discomfort, skin flare-ups, joint stiffness, or recurring inflammation often see improvements because functional medicine looks at the whole body, not just the affected organ.
What Kind of Results Can I Expect in 90 Days?
Ninety days is generally enough time for patients to experience a noticeable reduction in flare-ups, better sleep, improved digestion, balanced energy, and more stable lab values. While complete reversal takes time and varies from person to person, most people feel more in control of their health and see their symptoms becoming less intense and less frequent.
Do I Need to Stop My Current Medications?
No. Functional medicine works alongside conventional treatment. Medications should never be stopped without medical supervision. Over time, as the body stabilises and inflammation reduces, some individuals are able to lower their dosages—but only under the guidance of their primary doctor.
Why Are Autoimmune Diseases Increasing So Fast in India?
A combination of factors—processed foods, sedentary routines, pollution, chronic stress, gut imbalance, and nutrient deficiencies—are placing extra strain on the immune system. Women are especially affected because of hormonal fluctuations and higher exposure to certain lifestyle stressors. Functional medicine addresses these everyday triggers that conventional care often overlooks
What Does a Functional Medicine Plan Typically Include?
A functional medicine protocol usually begins with a detailed assessment and advanced testing. This is followed by a nutrient-rich, anti-inflammatory food plan, gut-healing support, detoxification guidance, stress and sleep optimisation, and personalised supplements where needed. The plan evolves over 90 days based on the individual’s progress and lab results, making it highly customised.
How Do I Choose the Right Functional Medicine Practitioner?
A trustworthy practitioner will have recognised training, experience with autoimmune cases, and a clear diagnostic approach. They will offer personalised nutrition and lifestyle support instead of relying heavily on supplements. They should also be transparent about your timeline, costs, and expected results, and encourage coordination with your existing healthcare providers.
Final Takeaway
Autoimmune conditions pose serious challenges—but they also respond differently when treated via root-cause, system-based care. In India, where lifestyle, environment, and nutrition often conspire against immune balance, a 90-day functional-medicine framework offers a clear path to improvement: symptom reduction, immune stabilisation, and lifestyle transformation. If you’re living with autoimmunity and feeling stuck in reactive treatment cycles—this approach may help you move toward true healing, not just management.
References
- “Functional, Bio Regulatory Medicine is the advanced version.” ET HealthWorld
- “Yoga in autoimmune disorders: a systematic review of RCTs.” PubMed. 2025.
- “Autoimmune Disease Treatment with Functional Medicine” – Freedom Age (India). February 2025.
- “Functional Medicine for Autoimmune Disease Management” -Revital Trichology & Wellness.
- “What is Functional Medicine India?” -Doctor Anjali Hooda Sangwan, LiveNutrifit.
- Roy S, Bagchi B. “Vitamin D sensitivity to the immune responses and autoimmunity: ArXiv
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset