Table of Contents
In today’s fast-paced world, many of us feel stretched in more ways than one: juggling work, family, city life, endless screen time, and diet changes. When the mind is under pressure, the body often follows – manifesting as hormonal imbalance, immune dysregulation (over or under reactive), low energy, respiratory flare-ups or chronic pain. But what if one of the most powerful healing tools is both ancient and modern — and bridges mind, body, and science?
Enter the union of Yoga and Functional Medicine. In this article, we explore how they form a perfect healing pair, especially in India’s unique context, and how this combo may benefit respiratory conditions, metabolic conditions, chronic conditions, hormonal imbalances, and autoimmune conditions through a root-cause, systems-based approach.
Why Functional Medicine in India Matters
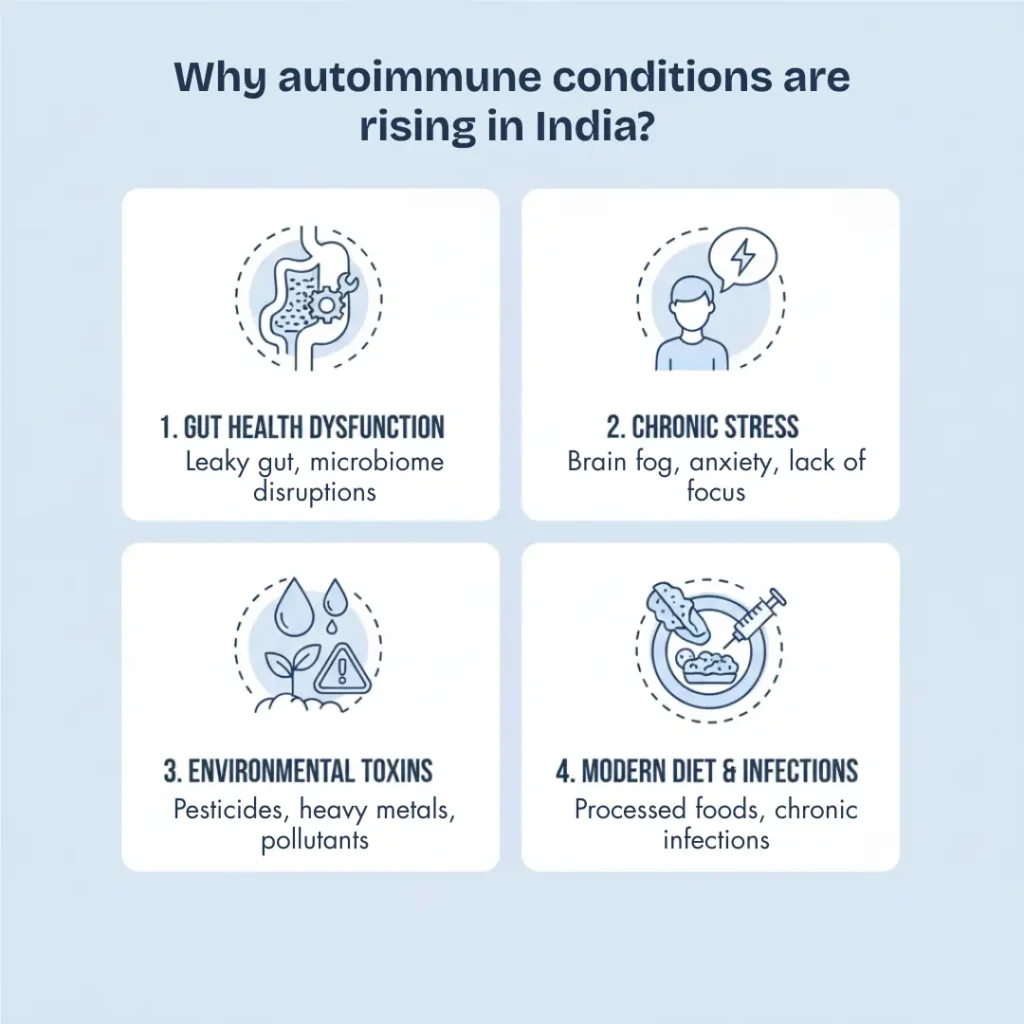
Functional medicine is a systems biology-based, patient-centred approach that focuses on identifying and addressing the root causes of disease rather than merely managing symptoms. It asks not only what is wrong, but why it happened. In India, where metabolic disease, pollution, stress, and autoimmune conditions are rising, this approach is increasingly relevant.
For example, patients with thyroid autoimmunity may be told, “your TSH is elevated — take levothyroxine” — but functional medicine would ask: Why is the TSH elevated? Is there an autoimmune attack on the thyroid tissue? What is triggering this immune attack on your thyroid? Is cortisol dysregulated? Is the gut barrier compromised? Are environmental toxins or lifestyle stress playing a role? This deeper lens can point to long-term improvement.
By combining this with Yoga — an embodied practice rooted in Indian tradition — you get a synergy of modern systems thinking + time-tested mind-body technique. That’s the “perfect healing pair”.
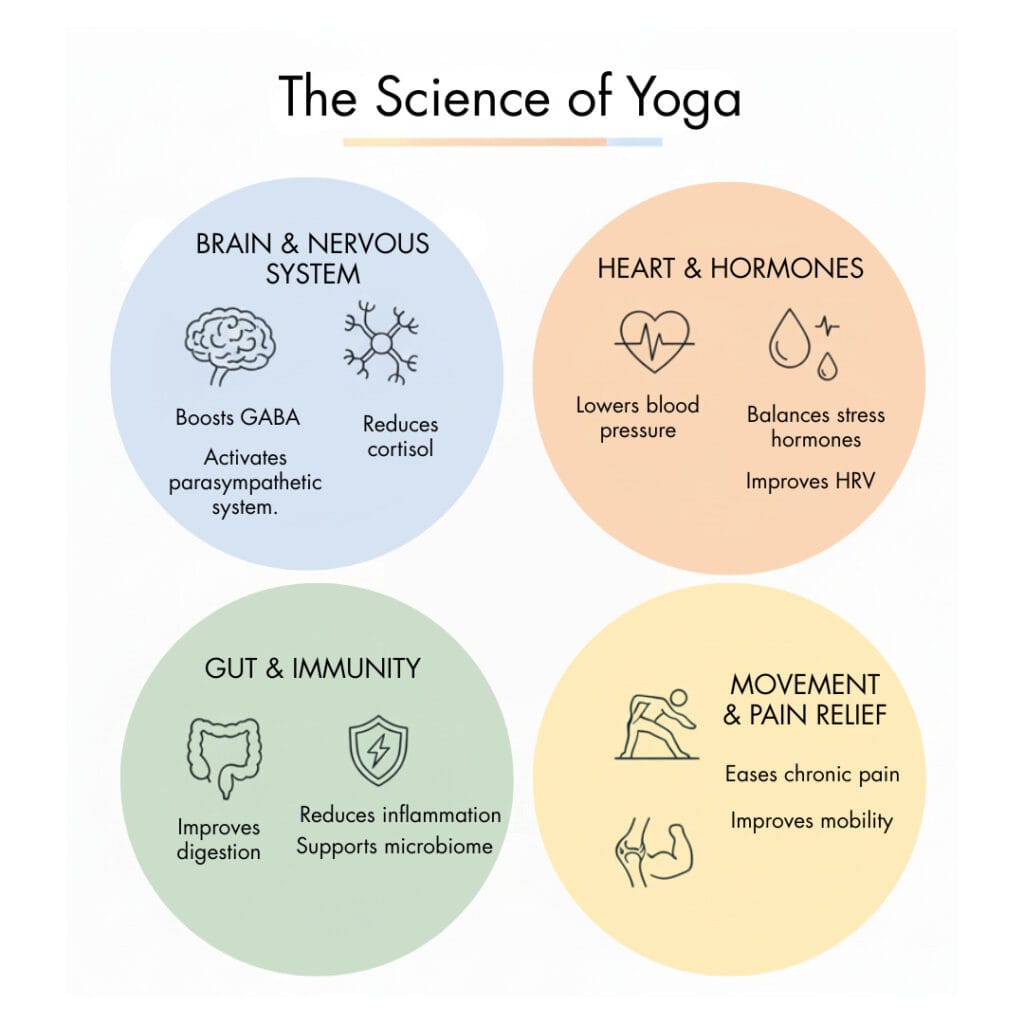
The Science of Yoga: More Than Flexibility
Yoga isn’t just stretching and breathing — it is a therapeutic tool for balancing, activating and rejuvenating the nervous, endocrine, immune, and musculoskeletal systems.
Several studies support this:
- A randomized controlled trial in female patients with multiple sclerosis found yoga training (90 min, 3 days/week for 8 weeks) led to a significant reduction in cortisol and modulation of ACTH compared to controls. PubMed
- In medical students in India, a yoga + meditation intervention significantly lowered salivary or serum cortisol levels, indicating reduced stress-hormone activation. MSJ Online+1
- A systematic review of yoga for gastrointestinal disorders found that yoga improved symptom severity, mood-related symptoms, and quality of life in chronic gut-brain interaction disorders — showing yoga’s reach into immune, endocrine, and gut systems. PubMed
- A meta-analysis on power vs stretch yoga found significant cortisol reductions after yoga sessions, showing even a single-session benefit for hormonal/ stress balance. PubMed
These studies show how Yoga influences cortisol, the major stress hormone, and by extension affects hormonal balance, immune regulation, and systemic health.
How Functional Medicine and Yoga Complement Each Other
When you map how stress → cortisol → hormone/immune disruption works, you see where yoga and functional medicine meet.
| Functional Medicine Focus | How Yoga Supports It |
| Identifying cortisol dysregulation, gut-immune-hormone interactions, and environmental/lifestyle load | Yoga down-regulates the HPA axis, lowers cortisol, improves autonomic balance, and enhances vagal tone |
| Modulating immune responses, balancing hormones (thyroid, female/male, adrenal) | Yoga improves hormone sensitivity, lowers inflammation, and supports restful recovery |
| Addressing lifestyle factors (sleep, diet, pollutant exposures, sedentary behaviour) | Yoga encourages whole-body movement, breath awareness, and mindfulness, and helps regulate sleep and stress |
| Offering sustainable practices beyond pills/supplements | Yoga offers self-empowering skills, accessible in India, scalable for many conditions |
In practice: A functional medicine practitioner in India might recommend lab tests (cortisol rhythm, nutrient panels, thyroid/adrenal hormones), tailor nutrition and lifestyle plans, and incorporate yoga (asana + pranayama + meditation) as a primary modality for stress and hormone regulation.
Conditions Where This Pairing Shows Promise
Respiratory Conditions
Chronic respiratory conditions (asthma, COPD, allergic rhinitis) have strong links with immune dysregulation, inflammation, and stress. Yoga helps reduce airway reactivity, improve breathing mechanics, and down-regulate stress response (cortisol/immune). Functional medicine adds root-cause work (e.g., gut-lung axis, toxin exposure, nutrient deficits) for a fuller solution.
Metabolic Conditions
Conditions like type 2 diabetes, insulin resistance, PCOS, and obesity are epidemic in India. Elevated cortisol increases insulin resistance; poor sleep and chronic stress amplify metabolic dysfunction. Yoga lowers cortisol, improves insulin sensitivity, and supports metabolic health. Functional medicine adds targeted nutrition, supplement/lab testing, and lifestyle interventions to support hormone/metabolic balance.
Chronic Conditions
Chronic fatigue, pain syndromes, fibromyalgia, and long-term low-grade inflammation often share hormonal and immune imbalances. Yoga supports autonomic regulation, improves vagal tone, and reduces stress impact. Functional medicine maps out root causes (toxins, nutrient gaps, gut/immune dysfunction) and builds personalised healing.
Autoimmune Conditions
Autoimmune conditions (thyroid disease, RA, lupus, psoriasis) involve misregulation of the immune system. Chronic stress + high cortisol disrupts immune tolerance. Yoga helps modulate the HPA axis, lower cortisol and improve immune-nervous system coordination. Functional medicine investigates underlying triggers (gut permeability, nutrient deficiencies, toxin/microbe load, hormonal dysbalance) and designs long-term support.
A Practical Framework: 90-Day Integration Strategy
To bring this into actionable terms, here is a 90-day roadmap pairing yoga + functional medicine principles:
Days 1-30 – Stress Reset
- Begin daily yoga practice (20-30 min) focusing on gentle asanas, Pranayama (breathwork), and meditation.
- Functional medicine: Baseline labs (cortisol rhythm, thyroid/adrenal panel, nutrient panel, gut markers). Diet: stabilise meals, remove refined carbs, and processed foods. Sleep hygiene. Environmental assessment (pollution/home exposures).
Days 31-60 – Rebuild & Rebalance
- Increase yoga intensity gradually (include poses focusing on core strength, hip openers, restorative yoga).
- Functional medicine: Nutrient repletion (Vit D, magnesium, zinc, omega-3), gut repair protocol. Address hormonal panels (thyroid/adrenals), integrate movement (strength training + yoga). Continue sleep/stress/lifestyle optimisation.
Days 61-90 – Restore & Maintain
- Deepen the yoga practice: integrate more mindfulness, longer holds, restorative sessions, and community- and teacher-led classes.
- Functional medicine: Review labs, adjust protocols, build a maintenance plan, and integrate periodic check-ins. Emphasise sustainability and lifestyle as medicine.
By day 90, many individuals may see improved cortisol rhythm, better sleep, reduced flare-ups, improved mood, and better hormonal/metabolic markers — though individual results vary.
Frequently Asked Questions (FAQs): Yoga & Functional Medicine
1. How do Yoga and Functional Medicine work together for healing?
Yoga helps regulate stress, nervous system balance, and hormonal responses, while Functional Medicine identifies and addresses underlying root causes such as inflammation, nutrient deficiencies, gut issues, and hormonal imbalances. Together, they support whole-body healing rather than symptom-only relief.
2. Is Yoga alone enough to manage chronic or autoimmune conditions?
Yoga is a powerful supportive practice, especially for stress reduction and nervous system regulation. However, chronic and autoimmune conditions often have multiple root triggers. Functional Medicine complements yoga by addressing biochemical, nutritional, hormonal, and environmental factors that yoga alone may not resolve.
3. Can this approach help with stress-related hormonal imbalances?
Yes. Chronic stress disrupts cortisol and other hormones. Yoga helps down-regulate the stress response, while Functional Medicine evaluates cortisol rhythm, thyroid, adrenal, and sex hormones to create a targeted plan for restoring balance.
4. How is this approach relevant in the Indian context?
India faces rising levels of metabolic disease, pollution exposure, stress, and autoimmune conditions. Yoga is culturally accessible and affordable, while Functional Medicine offers personalised, root-cause-based care—making this combination especially relevant and sustainable.
5. What conditions may benefit most from combining Yoga and Functional Medicine?
This integrated approach shows promise for respiratory conditions (like asthma), metabolic disorders (diabetes, PCOS), hormonal imbalances, chronic fatigue and pain syndromes, and autoimmune conditions such as thyroid disorders and rheumatoid arthritis.
6. How long does it take to see results with this combined approach?
Results vary by individual. Many people notice improvements in sleep, energy, stress tolerance, and symptom flare-ups within 8–12 weeks when yoga is practiced consistently and Functional Medicine protocols are followed under guidance.
7. Is this approach meant to replace conventional medical treatment?
No. Yoga and Functional Medicine are complementary approaches. They work best alongside conventional care, especially for diagnosis and acute management, while focusing on long-term healing, resilience, and prevention.
8. What is the first step to begin integrating Yoga and Functional Medicine?
Start with a consistent, gentle yoga routine focused on breath and relaxation. At the same time, consult a qualified Functional Medicine practitioner to assess root causes and create a personalised nutrition, lifestyle, and testing plan.
Final Thoughts
Yoga and Functional Medicine form a potentially powerful pairing: one rooted in ancient mind-body wisdom, the other grounded in modern systems medicine. Together, especially in the Indian context where stress, metabolic, hormonal, and immune burdens are high, they offer a path of healing that goes beyond symptom management — toward system regulation and resilience.
If you’re managing a respiratory, metabolic, chronic or autoimmune condition, consider this integrated path. Ask your practitioner about cortisol/hormone testing, integrate a consistent yoga practice, and adopt supportive lifestyle changes. Healing isn’t always instant. But with consistency, you may move from chaos toward balance.
References
- “The effect of yoga training on the enhancement of Adrenocorticotropic hormone (ACTH) and cortisol levels in female patients with Multiple Sclerosis.”-PubMed
- “Effect of yoga on salivary cortisol.”-MSJ Online
- “The effect of yoga training on enhancement of Adrenocorticotropic hormone” -National Library of Medicine
- “A systematic review of yoga for the treatment of gastrointestinal disorders.”-PubMed.
Please subscribe to our social channels for updates related to functional medicines.
Instagram: thehormonereset
Facebook: Hormone Reset
YouTube: Hormone Reset Program
LinkedIn: Hormone Reset